Alzheimer’s & Brain Awareness Month 2020
Worldwide, 50 million people are living with Alzheimer's and other dementias. Every June, the Alzheimer's Association raises awareness of this neurodegenerative disease during Alzheimer’s & Brain Awareness Month. The American Society for Biochemistry and Molecular Biology participated in this effort by sharing recent studies of interest to patients, caregivers and researchers.
What is Alzheimer’s?
Alzheimer's disease is a type of dementia that causes problems with memory, thinking and behavior. The disease is named after Alois Alzheimer. In 1906, he noticed changes in the brain tissue of a woman who had died of an unusual mental illness. Her symptoms included memory loss, language problems and unpredictable behavior. After she died, he examined her brain and found many abnormal clumps (now called amyloid plaques) and tangled bundles of fibers (now called neurofibrillary, or tau, tangles).
According to the Alzheimer’s Association, Alzheimer's disease accounts for 60% to 80% of dementia cases. Symptoms usually develop slowly and get worse over time, becoming severe enough to interfere with daily tasks.
There is no cure yet for Alzheimer's, but treatments can temporarily slow the worsening of symptoms and improve quality of life for patients and their caregivers. Treatment addresses several different areas: maintaining mental function, managing behavioral symptoms, and slowing or delaying symptoms.
A recent article in the journal Alzheimer’s & Dementia reported that, in 2014, an estimated 5 million Americans 65 years or older had Alzheimer’s disease, and this number is projected to nearly triple to 14 million people by 2060. In the New England Journal of Medicine, researchers reported that, in 2010, the costs of treating Alzheimer’s disease were projected to fall between $159 billion and $215 billion. Moreover, by 2040, these costs are projected to jump to between $379 billion and more than $500 billion annually.
How is it diagnosed?
Alzheimer’s disease is not a normal part of aging. The most common early symptom is difficulty remembering newly learned information. Changes typically begin in the part of the brain that affects learning. According to the National Institute of Aging, people with Alzheimer’s have trouble doing everyday things, such as driving a car, cooking a meal or paying bills. They may ask the same questions over and over, get lost easily, lose things or put them in odd places, and find even simple things confusing. As the disease progresses, some people become worried, angry or violent.
As Alzheimer's advances through the brain, it leads to increasingly severe symptoms, including disorientation; mood and behavior changes; deepening confusion about events, time and place; unfounded suspicions about family, friends and professional caregivers; more serious memory loss and behavior changes; and difficulty speaking, swallowing and walking.
What are risk factors and common causes?
The disease likely develops from multiple factors, such as genetics, lifestyle and environment.
The greatest known risk factor is increasing age. The majority of people with Alzheimer's are 65 and older. About 200,000 Americans under the age of 65 have early-onset Alzheimer’s disease.
Another strong risk factor is family history, according to the Centers for Disease Control and Prevention. The two categories of genes that influence whether a person develops Alzheimer's are risk genes and deterministic genes. Less than 1% of Alzheimer’s cases are caused by deterministic genes (genes that cause a disease, rather than increase the risk of developing a disease).
What are researchers doing?
Today, researchers are working to uncover as many aspects of Alzheimer's disease and other dementias as possible through studies examining various facets of the disease. Below are recent articles about Alzheimer's in ASBMB journals.
Impaired tau–microtubule interactions are prevalent among pathogenic tau variants arising from missense mutations
One of the hallmarks of Alzheimer's disease and other similar disorders is the aggregation of tau proteins into pathological inclusions. The tau protein promotes tubulin assembly and stabilizes microtubules by binding longitudinally along the microtubule surface. This study shows that only a few tau variants are intrinsically prone to this type of aggregation, and microtubule-targeting therapies might be effective in the management of disease due to the deposition of abnormal tau protein in the brain.
CD2AP overexpression accelerates APP transfer from early endosomes to the lysosomal degradation pathway
Another hallmark of Alzheimer's disease is the appearance of senile plaques, composed of β-amyloid (Aβ) peptides. Aβ is produced by sequential cleavages of amyloid precursor protein (APP) by β- and γ-secretases during intracellular trafficking through the endocytic and recycling pathways. One of the risk factors for late-onset AD is CD2-associated protein (CD2AP), an adaptor molecule that regulates membrane trafficking. The authors of this study sought to understand how CD2AP regulates APP trafficking. They found that CD2AP accelerates the transfer of APP from early to late endosomes and stimulates APP degradation, which may explain why impaired CD2AP function is a risk factor for Alzheimer's.
Endoplasmic reticulum stress responses in mouse models of Alzheimer's disease
Endoplasmic reticulum (ER) stress is also believed to play a role in Alzheimer's disease (AD). However, whether ER stress is caused by AD pathology is unclear. This study suggests that ER stress is also not essential in tau pathology–induced neurodegeneration, therefore the role of ER stress in AD pathogenesis needs to be carefully addressed in future studies.
What can proteomics tell us about the Alzheimer's brain?
Alzheimer′s disease is becoming more prevalent in aging populations. Proteomics can improve early diagnosis and treatment by providing insights into disease etiology and possible treatment avenues. This review article explores how proteomics studies have contributed to the development of biomarkers for clinical diagnostics, and the recognition of proteins that can help elucidate the pathways leading to AD brain pathology.
Modeling of pathological traits in Alzheimer's based on systemic extracellular signaling proteome
Studying Alzheimer's disease in patients is typically limited to brain imaging or psychometric testing. New tools, however, are identifying the molecular changes underlying this disease. The authors of this study found small numbers of signaling proteins that can model key pathological markers of Alzheimer's disease, and leads to the implication of novel signaling pathways in this disorder.
An interactive literature guide to quantitative cerebrospinal fluid mass spectrometry data from neurodegenerative disorders
There is a need for organizing biomedical proteomics information in a way that is available to the research community. This work investigated scientific publications describing the analysis of the cerebrospinal fluid proteome in relation to multiple sclerosis, Parkinson's disease and Alzheimer's disease. Cerebrospinal fluid is considered to be the most attractive body fluid in the search for biomarkers related to neurological disorders. The resulting dataset (CSF-PR 2.0) included novel approaches for filtering, visualizing and comparing quantitative proteomics information for quantitative proteomics on cerebrospinal fluid.
Cholesterol: from heart attacks to Alzheimer's disease
One of the contributing factors to Alzheimer's disease is the aggregation of the amyloid-β peptide (Aβ) in the brain. Therefore, blocking the generation of Aβ is a potentially important treatment strategy. Cholesterol has recently been associated with the processing of Aβ and may have the potential to affect AD. Read more.
Role of LRP1 in the pathogenesis of Alzheimer’s disease
Accumulating evidence from preclinical studies indicates that one of the low-density lipoprotein receptor (LDL) family members, LDLR-related protein 1, has a role in the pathogenesis of Alzheimer’s disease. LRP1 regulates the metabolism of amyloid-β peptides in the brain. Yet, evidence from clinical studies is not sufficient to conclude how LRP1 contributes to Alzheimer's development. This review discusses the potential mechanisms underlying how LRP1 affects Alzheimer's pathogenesis through Aβ-dependent and -independent pathways, as well as potential therapeutic strategies for targeting LRP1.
Ketone body therapy: from the ketogenic diet to the oral administration of ketone ester
The brain readily utilizes ketone bodies as an alternative to using glucose for energy. Upon diminished glucose utilization in cognition-critical brain areas, such as early in Alzheimer’s disease, these areas can still metabolize ketone bodies. Particular esters can produce plasma ketone levels comparable to those achieved by the most rigorous ketogenic diet, providing a new approach to the study and potential treatment of a variety of diseases, including Alzheimer's. Read the paper.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

The data that did not fit
Brent Stockwell’s perseverance and work on the small molecule erastin led to the identification of ferroptosis, a regulated form of cell death with implications for cancer, neurodegeneration and infection.

Building a career in nutrition across continents
Driven by past women in science, Kazi Sarjana Safain left Bangladesh and pursued a scientific career in the U.S.
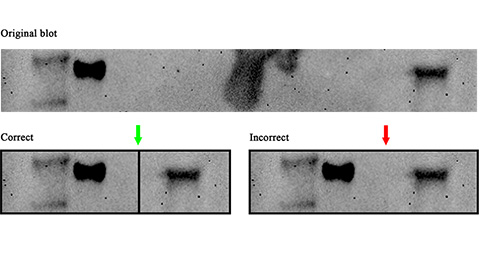
Avoiding common figure errors in manuscript submissions
The three figure issues most often flagged during JBC’s data integrity review are background signal errors, image reuse and undeclared splicing errors. Learn how to avoid these and prevent mistakes that could impede publication.
Ragweed compound thwarts aggressive bladder and breast cancers
Scientists from the University of Michigan reveal the mechanism of action of ambrosin, a compound from ragweed, selectively attacks advanced bladder and breast cancer cells in cell-based models, highlighting its potential to treat advanced tumors.
Lipid-lowering therapies could help treat IBD
Genetic evidence shows that drugs that reduce cholesterol or triglyceride levels can either raise or lower inflammatory bowel disease risk by altering gut microbes and immune signaling.
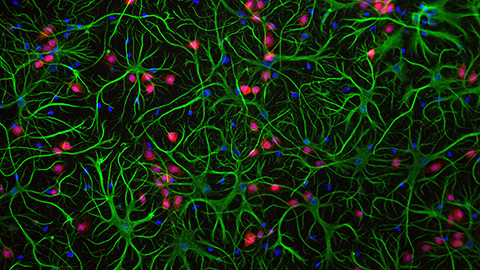
Key regulator of cholesterol protects against Alzheimer’s disease
A new study identifies oxysterol-binding protein-related protein 6 as a central controller of brain cholesterol balance, with protective effects against Alzheimer’s-related neurodegeneration.

