Finding a way to combat long COVID
A new study has identified potential neurological biomarkers of long COVID-19 in nonhuman primates that may help physicians diagnose, monitor and treat this condition.
Over 65 million people worldwide have developed long COVID after being infected with SARS-CoV-2, and cases are only becoming more common. Long COVID symptoms can last weeks, months or years. Even more perplexing is the fact that symptoms can vary widely between individuals and consist of any combination of fatigue, fever, chest pain, trouble breathing, neurological symptoms such as “brain fog,” and many more. Long COVID puts a gigantic burden on the U.S. healthcare system, and some doctors doubt the condition exists, leaving some patients unable to find care.
A team of researchers at Tulane University is trying to shed light on this condition and find tools to manage it. They published their work in the journal Molecular & Cellular Proteomics.
“Our primary goal was to better understand the inside of the brain after COVID infection,” said Jia Fan, an assistant professor of biochemistry and molecular biology who oversaw the study. “This understanding could provide a potential target to use in the clinic for long COVID evaluation and monitoring. We also thought this study may give us some clues to find a potential treatment strategy for long COVID in patients.”
However, because long COVID can vary drastically between individuals, studying this disorder has been difficult for scientists and clinicians alike.
“There's a very limited understanding of the neuropathogenesis of long COVID,” Fan said. “It is almost impossible to get any brain tissue or samples of any kind from patients that have mild symptoms or no long COVID symptoms because there is no reason for invasive procedures.”
Therefore, the group turned to a nonhuman primate model of long COVID. They used two different types of nonhuman primates, the rhesus macaque and the African green monkey, to mimic the genetic differences seen in humans.
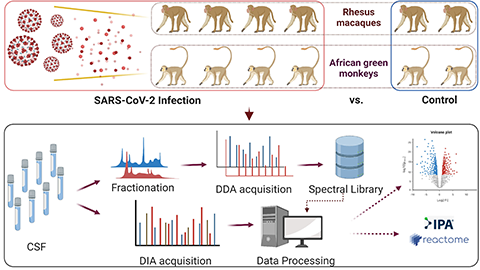
“Macaques are bred in captivity,” Sudipa Maity, a postdoctoral fellow at Tulane and lead author of the study, said. “So, they are born, fed and live their entire life in the research center. They also have very similar genetic backgrounds. On the contrary, the African green monkeys live in the wild and are brought to the center around one year before the study. Therefore, the individual genetic variations are larger in the African green monkey than the rhesus macaque.”
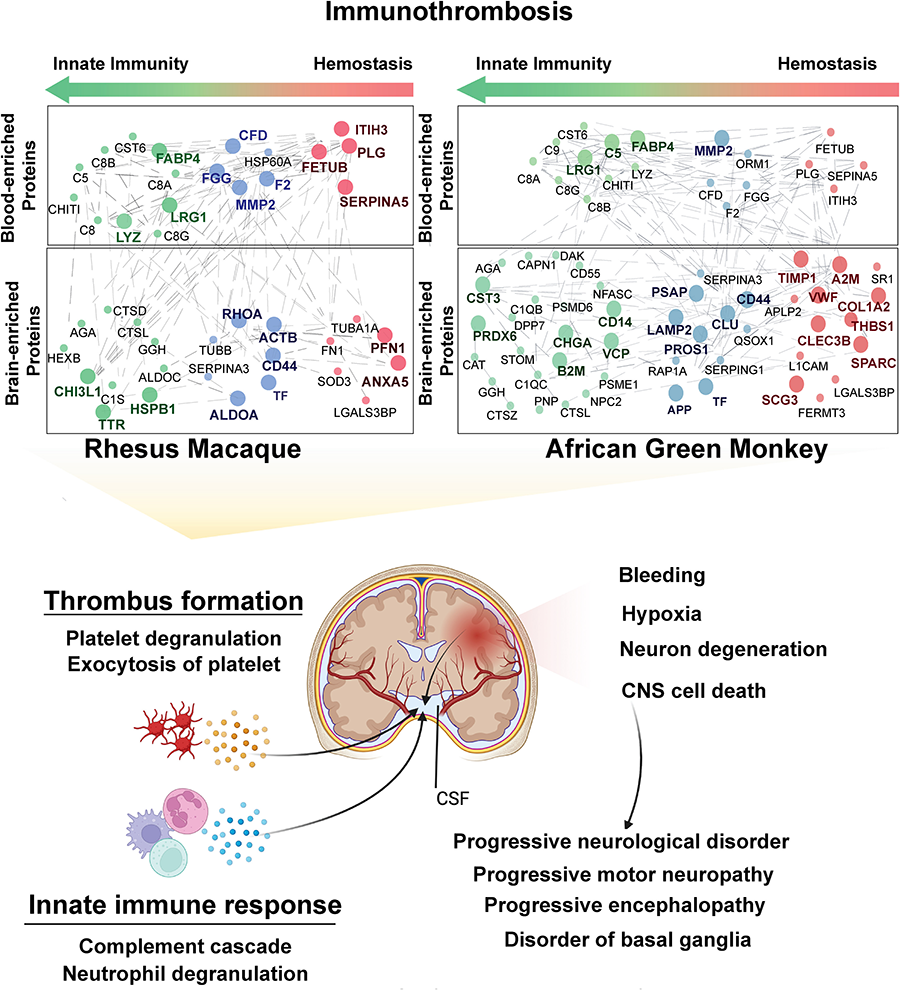
The team found that certain proteins associated with neurodegenerative disorders, such as Parkinson's disease, were elevated in the brain, cerebrospinal fluid and blood after SARS-CoV-2 infection even in nonhuman primates that showed mild or no symptoms. Maity explained that these elevated proteins indicate that the immune systems of the monkeys remained activated even after infection.
“Our findings suggest that the major neurological complications are arising due to the body's natural immune defenses,” Maity said. “The immune system has a very important and significant impact on the neurological complications of COVID.”
The next steps of the project involve validating the biomarkers the team identified in human samples such as blood, said Fan.
“It is currently hard to score the severity of (long COVID) patient symptoms because they are based on self-reports,” Fan said. “If we can find a group of proteins in the blood associated with long COVID, this is a less invasive way to easily evaluate the severity of the long COVID patients. We hope what we started can provide a clue to find a potential treatment to better the long COVID patient experience.”
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

Targeting Toxoplasma parasites and their protein accomplices
Researchers identify that a Toxoplasma gondii enzyme drives parasite's survival. Read more about this recent study from the Journal of Lipid Research.

Scavenger protein receptor aids the transport of lipoproteins
Scientists elucidated how two major splice variants of scavenger receptors affect cellular localization in endothelial cells. Read more about this recent study from the Journal of Lipid Research.

Fat cells are a culprit in osteoporosis
Scientists reveal that lipid transfer from bone marrow adipocytes to osteoblasts impairs bone formation by downregulating osteogenic proteins and inducing ferroptosis. Read more about this recent study from the Journal of Lipid Research.

Unraveling oncogenesis: What makes cancer tick?
Learn about the ASBMB 2025 symposium on oncogenic hubs: chromatin regulatory and transcriptional complexes in cancer.

Exploring lipid metabolism: A journey through time and innovation
Recent lipid metabolism research has unveiled critical insights into lipid–protein interactions, offering potential therapeutic targets for metabolic and neurodegenerative diseases. Check out the latest in lipid science at the ASBMB annual meeting.

Melissa Moore to speak at ASBMB 2025
Richard Silverman and Melissa Moore are the featured speakers at the ASBMB annual meeting to be held April 12-15 in Chicago.

