Innovative approach opens the door to COVID nanobody therapies
COVID is not yet under control. Despite a bevy of vaccines, monoclonal antibodies, and antivirals, the virus continues to mutate and elude us. One solution that scientists have been exploring since the early days of the pandemic may come in the form of tiny antibodies derived from llamas, which target various parts of the SARS-CoV-2 spike protein.
In a new study in the Journal of Biological Chemistry, researchers describe a less expensive way to isolate and identify these so-called nanobodies. The findings will make it easier for scientists around the world to try their hand at discovering nanobodies that target SARS-CoV-2 or other viruses. “Our method is more straightforward and less expensive than existing techniques,” says Rockefeller’s Michael P. Rout. “You do need a llama, but that — along with all the most complicated parts of the process — can be outsourced.”
The authors have already used this optimized method to identify multiple nanobodies that appear to work against key variants of the virus, including omicron. “COVID is clearly going to be a problem for some time,” Rout says. “We show that many of the nanobodies we have identified with this method target variants-of-concern, so they have real therapeutic potential.”
Nanobody novelty
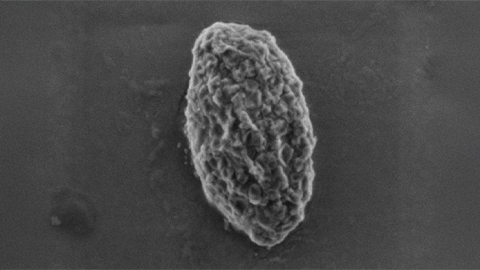
Nanobodies may work where larger antibodies fail, in part due to their compact size. Studies have shown that nanobodies can squeeze into parts of the SARS-CoV-2 virus that larger antibodies cannot reach. Nanobodies also have unusually long shelf-lives, cost very little to mass-produce and, because of their unique physical properties, could theoretically be inhaled.
Camelids such as llamas naturally produce nanobodies when exposed to a virus, and Rout and colleagues have developed enormous libraries of promising SARS-CoV-2 nanobodies by giving a small dose of COVID protein to llamas (which produce nanobodies in response, much as humans produce antibodies in response to a vaccine). After taking small blood samples from the llamas and sequencing the nanobody DNA, the scientists later transfer key genes to bacteria which, in turn, produce many more nanobodies for lab analysis.
But screening these nanobody libraries to see how well they work (and which variants they work against) can be time-consuming and expensive. Rout and colleagues have long relied on the “mass spectrometry” technique, which works extraordinarily well but requires substantial expertise to perform and expensive equipment. They wondered whether a recently discovered “yeast display method”, which was potentially far less expensive and simpler, could also effectively sort through their nanobody library.
Rout, in collaboration with Rockefeller’s Fred Cross, started by first optimizing the yeast display method. (The two heads-of-lab took the unusual step of performing most of the benchwork themselves). They then used their optimized method to screen a library of nanobodies that they had previously screened with the mass spectrometry technique. They found that their version of the yeast display method not only identified many of the same nanobody candidates as the other approach, but also identified numerous other candidates that they had missed.
“The method is not ours,” Cross clarifies. “But we made it simpler.”
Toward nanobody therapy
The relatively simple and low-cost procedure described in the paper could empower laboratories in low-resource areas to generate nanobodies against SARS-CoV-2, as well as other viruses. “A researcher anywhere in the world, with fairly limited resources, could use this technique,” Rout says. “The llama-related stuff could be FedEx-ed from North America.”
For COVID, the long-term goal is that techniques such as these will lower the bar for entry into nanobody research and ultimately produce therapies that prevent infection. “How we’d make the therapeutic is unestablished, as yet,” Cross says. “The specificity is there and the activity is there, but we don’t have a drug yet. It’d be nice if we did. Hopefully someday.”
Because with COVID now transitioning to an endemic disease, novel methods for preventing the infection cannot come soon enough. “New variants become prevalent by evading the immune system,” Cross says. “It’s important to have a fast way to find new nanobodies targeting the variants.”
This article was first published by The Rockefeller University. Read the original.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

RA patient blood reveals joint innerworkings
Researchers in the Netherlands use mass spectrometry to compare the proteome of plasma and synovial fluid in rheumatoid arthritis patients and find a correlation. Read more about this recent paper in Molecular & Cellular Proteomics.

Hope for a cure hangs on research
Amid drastic proposed cuts to biomedical research, rare disease families like Hailey Adkisson’s fight for survival and hope. Without funding, science can’t “catch up” to help the patients who need it most.

Before we’ve lost what we can’t rebuild: Hope for prion disease
Sonia Vallabh and Eric Minikel, a husband-and-wife team racing to cure prion disease, helped develop ION717, an antisense oligonucleotide treatment now in clinical trials. Their mission is personal — and just getting started.

Defeating deletions and duplications
Promising therapeutics for chromosome 15 rare neurodevelopmental disorders, including Angelman syndrome, Dup15q syndrome and Prader–Willi syndrome.
Using 'nature’s mistakes' as a window into Lafora disease
After years of heartbreak, Lafora disease families are fueling glycogen storage research breakthroughs, helping develop therapies that may treat not only Lafora but other related neurological disorders.
Cracking cancer’s code through functional connections
A machine learning–derived protein cofunction network is transforming how scientists understand and uncover relationships between proteins in cancer.

