Vitamin D: How much is enough?
Her body hurt. It wasn’t the ache of tired bone and muscle after a long day but severe musculoskeletal pain that had been progressing over five years. The 35-year-old woman underwent extensive medical workups, which resulted in her being offered narcotics and antidepressants. She declined those. She even had a bone scan that showed abnormalities that no one could explain. Finally, the day came when the pain weakened the woman to the point that she couldn’t stand at the kitchen counter. Her children were taken away from her because she was unable to fulfill her parental duties.
Then she showed up in Gregory Plotnikoff’s office at Allina Health Care in Minneapolis. He noted that the woman had trouble getting up from a chair and the bone abnormalities recorded in her medical reports. He ordered a vitamin-D test. The test results showed that she was profoundly deficient in vitamin D, so he prescribed her supplements. “Truly, $100 worth of vitamin D, and she got her two kids back,” he says.
Plotnikoff brings up this anecdote when he argues that we, as a population, need to increase our intake of vitamin D. He is one of several clinicians who are convinced that an unrecognized vitamin-D deficiency is the root of a slew of illnesses that are not limited to only bone. They include cardiovascular disease, various cancers and autoimmune disorders. They say that the current recommendation by the Institute of Medicine that everyone, from toddlers to the elderly, take 600 international units of vitamin D every day is woefully inadequate.
Other experts disagree. They say that there is solid evidence to connect vitamin D only to bone health, on which the IOM based its recommendation in 2011. “There’s this view that vitamin D is a miracle hormone that does literally everything,” says J. Wesley Pike at the University of Wisconsin-Madison. “The fact of the matter is that’s just simply not true.”
What is vitamin D?
There are two types of vitamin D: vitamin D2 and vitamin D3. Vitamin D2 is generally found in fortified foods, such as milk and some other dairy products, cereals and orange juice. The few natural sources of vitamin D include shitake mushrooms and fatty fish, such as salmon, sardines and mackerel. Vitamin D3 is the product of sunshine. Ultraviolet light from the sun converts 7-dehydrocholesterol in the skin into previtamin D3. The previtamin D3 gets turned into vitamin D3.
But both forms of vitamin D need to be activated to work. Vitamin D2 and D3 get hydroxylated by a P450 enzyme in the liver to be turned into 25-hydroxyvitamin D. This prohormone binds to a protein in the blood called the serum vitamin D-binding protein. Clasped to its binding partner, the prohormone then travels through the blood circulation system for about two weeks. When the bound prohormone gets to the kidneys, an enzyme called CYP27B1 hydroxylase in the proximal tubular epithelial cells turns it into the active hormone 1α,25-dihydroxyvitamin D.
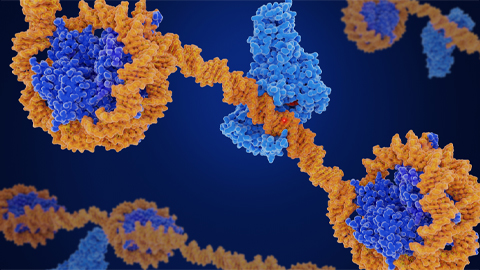
This active form of vitamin D has a fleeting existence in plasma. In the parathyroid gland, bone, kidney and intestine, 1α,25-dihydroxyvitamin D binds to the vitamin-D receptor, which is part of the nuclear receptor family of transcription factors. The transcription factor forms a heterodimer with the retinoid-X receptor. The heterodimer binds to hormone response elements on DNA to turn on or turn off the expression of a variety of genes, such as ones involved in calcium absorption in the intestine.

When is someone deficient?
Warped bones in children with rickets and adults with osteomalacia are signs of inadequate vitamin-D intake. In 1922, a group led by Elmer Verner McCollum at Johns Hopkins University demonstrated the existence of a fat-soluble nutrient that was involved in calcium absorption. They called this nutrient vitamin D. In 1924, Harry Steenbock and A. Black at the University of Wisconsin-Madison demonstrated that irradiating certain foods, most notably milk, and feeding those foods to animals reversed rickets. Steenbock patented his discovery, and the 1930s saw the introduction of foods fortified with vitamin D. By the end of the 1930s, rickets was no longer a public health problem.
The definition of a vitamin-D deficiency has morphed over time. Until the 1930s, rickets and osteomalacia were most the visible signs of the deficiency. These days, a deficiency in vitamin D is determined by a blood test. The test, usually based on an immunoassay, measures the level of the prohormone 25-hydroxyvitamin D. It’s clear that if someone has a blood level less than 20 ng/mL, that person is in danger of developing a bone disorder or hyperparathyroidism.
The IOM report in 2011 stated that a level between 21 ng/mL and 29 ng/mL of 25-hydroxyvitamin D was considered to be sufficient for maximum bone health. This is the range being disputed between vitamin-D experts. Some believe we need a blood level of more than 30 ng/mL of 25-hydroxyvitamin D; others think the IOM committee behind the report got it right.
The split comes over whether vitamin D does more than maintain bone health. Some experts think that vitamin D plays more roles than we give it credit for and that we should be taking higher doses of it so that it can do all its different physiological jobs. Other experts say the evidence for vitamin D in diseases beyond ones found in bone and parathyroidism is weak; they worry that higher doses may cause more harm than good.
The dispute actually has been going on for decades, and it was further fueled by the 2011 IOM report. Three years after the report, the debate hasn’t abated, as evidenced by two meta-analyses published in the British Journal of Medicine in April that attempted to make sense of the vitamin-D literature (see Theodoratou et al and Chowdhury et al). Based on the conclusions of the two studies, the BMJ editorial urged caution in attributing diseases (besides the ones in bone) to a vitamin-D deficiency.

The 2011 IOM report
The IOM report on vitamin D and calcium came about because “the federal agencies that make use of the dietary reference intakes were aware that there was the perception that the public might be becoming more vitamin-D deficient,” says A. Catharine Ross at Pennsylvania State University, who chaired the IOM committee for the 2011 report. Data were showing that clinicians and the public were increasingly shelling out money for vitamin D. In a New York Times story published in 2010, journalist Tara Parker Pope noted that in 2008, consumers spent $235 million on vitamin D supplements, compared with $40 million in 2001; orders by physicians for vitamin D tests with Quest Diagnostics dramatically rose in 2009.
So the IOM committee, sponsored by the U.S. Department of Agriculture, U.S. Department of Defense, U.S. Department of Health and Human Services, and Health Canada, was tasked with analyzing the vitamin-D literature and making appropriate recommendations that could be applied to the general North American population.
The committee had to follow a risk-assessment model. In that model, explains Ross, there has to be a causal link between the intake of a nutrient and a physiological outcome, such as a bone disorder. “If you don’t have solid evidence that A is causally related to B, then it becomes not appropriate to use it” for establishing a dietary reference intake, she says.
For cardiovascular disease, autoimmune disorders and cancer — physiological disorders suggested to be connected to a vitamin-D deficiency — the committee could not find causal links. “There is quite a bit of literature,” acknowledges Ross. “But some of it is of the type where an observation was made in a population with cardiovascular disease, and serum vitamin-D levels may have been measured and were a little bit low. But that’s not establishing a link.”
Ross says the only clinical outcome that the committee could see where vitamin D had a direct effect was bone health. The literature on that was more extensive and conclusive, so the committee used it to base its recommendation of a daily vitamin D intake of 600 IU.
“It wasn’t that we ignored the other studies. It wasn’t that we said they were uninteresting or they were not to be considered,” Ross says. But in the report, the committee described the problems it ran into in trying to find the connections between vitamin D and other health outcomes other than bone disease:
“These include the difficulty of isolating the effects of a single nutrient under investigation from the confounding effects of other nutrients and non-nutrient factors; the multi-factorial etiology of the chronic diseases the committee considered; the paucity of data from randomized controlled clinical trials, which typically provide the highest level of scientific evidence relevant for (daily recommended intake) development; and the mixed and inconclusive results from observational studies.”
Some vitamin-D experts say that the IOM’s need to see data from randomized controlled trials is misguided and bewildering. “They said there’s not sufficient evidence to suggest that vitamin D has any real effect outside of the skeletal system because there weren’t any appropriate randomized controlled trials,” says Bruce Hollis at the Medical University of South Carolina. “Randomized controlled trials were designed for drugs, not nutrients.”Both he and Robert Heaney of Creighton University say that randomized controlled trials in nutrition are not feasible in most cases. Vitamin D is an essential nutrient. To test its effects on a certain physiological outcome in a randomized controlled trial, a significantly large group of participants within the study would have to be denied all sources of vitamin D. But this kind of trial simply cannot be done for ethical reasons, explains Heaney, when you know you are depriving people of an essential nutrient. But then organizations like the IOM turn around and say they can’t make recommendations for a nutrient without data from randomized controlled trials.
“We’ve got a catch-22,” says Heaney. “Randomized trials are purely empirical, which is fine for drugs. They are foreign agents. But nutrients and hormones are not foreign agents. They are native to the body. They should be there.”
Critics of the IOM report had other bones to pick. One was the question of sun exposure. Sun-driven production of vitamin D is the most effective source of the nutrient. In the summer, a white person can make 10,000 IU after spending 30 minutes in the early-afternoon sun without sunscreen. But Ross explains that the committee couldn’t recommend that people catch more sun because of the relationship between skin cancer and ultraviolet light exposure. “We ended up saying we will try to specify a recommended daily intake in the absence of sun,” says Ross. “We realized there really is no such thing as absence of sun, but we called it minimal sunlight exposure.” She says the 600 IU recommended for vitamin D was made to maintain an adequate serum level of the vitamin even in the absence of sun “but knowing full well that, for many people, sun adds to that. Chances are their actual total exposure, considering both diet and sun, is actually higher.”
Meanwhile, experts point out that black people have different requirements for vitamin D and calcium; melanin absorbs UV light and interferes with its transmission into the skin, reducing the production of vitamin D. Also, black Americans tend to consume less dairy, which is usually fortified with vitamin D. As John Adams at the University of California, Los Angeles, explains, the first values for serum levels of vitamin D were established by studying white people. He says that, if we look at the U.S. population today, about 60 percent of the white population has a serum level of 25-hydroxyvitamin D of less than 30 ng/mL. “If you look at African-Americans who have a (25-hydroxyvitamin D) level less than 30 ng/mL,” says Adams, “it’s 95 percent of the population.”
Sun exposure at different latitudes is another aspect that clinicians say needs to be considered. Plotnikoff says that he and colleagues have observed that Southeast Asians moving from their home countries to higher latitudes in the Western Hemisphere develop cardiovascular diseases and autoimmune disorders like multiple sclerosis. In these studies, patients were shown to have low levels of 25-hydroxyvitamin D.
But Hector DeLuca at the University of Wisconsin-Madison counters those studies. DeLuca, who served as a consultant to the IOM committee, uses multiple sclerosis as an example. “There is clearly a relationship between sunlight and the incidence of this disease. It’s been known since, I think, 1964. You know what? There are other things that sunlight does besides produce vitamin D,” he says. “But because the vitamin D system is so well-known and we know that it’s very important for health, everyone focused on the idea that maybe vitamin D” has something to do with multiple sclerosis. DeLuca says subsequent studies have shown in animal models that a vitamin-D deficiency doesn’t cause multiple sclerosis.
The IOM report set the upper limit for taking vitamin D at 4,000 IU for adults and between 2,500 and 3,000 IU for children, based on their ages. Critics say the upper limit could have been higher. They point to a review that showed that doses of vitamin D up to 10,000 IU were not toxic.
But Ross explains, “We’re making recommendations that might have a shelf life of a decade or more. You have to be cautious under those circumstances. I think that really helps to explain why we stop at 4,000, even though some people might say you could take more and it wouldn’t be harmful. We were not so certain.”
Pike and Adams both point out that the production of the active vitamin-D hormone is tightly regulated. Popping more vitamin D supplements may not actually affect your level of active vitamin D. The prohormone may just wind up leaving your body through urine. “If you get out in the sunlight, particularly in the equator, and you have a lot of exposed skin, you can make 25,000 or even 50,000 units of vitamin D in an hour,” says Pike. “But it’s not active because it needs to be converted eventually to (1α,25 dihydroxyvitamin D), irrespective of how much you have. It’s very tightly controlled. That’s really the key to the vitamin-D system — the hormone is exquisitely regulated.”
Michael Holick at Boston University chaired the Endocrine Society’s committee on vitamin D. The goal was to provide guidance to clinicians for the prevention and treatment of vitamin-D deficiency; the IOM’s goal was to provide guidance for the general population. Holick defends the IOM committee, even though he doesn’t agree with its recommendation. (He too thinks that the recommended daily intake should have been higher.) “I think they did a great job because, believe it or not, what people don’t realize is before they met the actual recommendation for vitamin D in all children and adults was 200 units a day,” he says. “They now say no, no, no, it’s actually 600. To me, that’s a big change.”
In the meantime, everyone is waiting to see the results from a large-scale randomized trial now happening under the purview of the National Institutes of Health. The agency is supporting a long-term study of daily intake of vitamin D3 pills of 2,000 IU. Spearheaded by JoAnn Manson and Julie Buring at Harvard University-affiliated Brigham and Women’s Hospital, the trial is called the vitamin D and omega-3 trial, from which various letters have been plucked to give the trial the name VITAL.
VITAL is tracking 25,875 men and women across the U.S. The study participants are divided into four groups: One group is taking both vitamin D and omega-3 fatty acid capsules; one group is taking vitamin D and a placebo; one group is taking omega-3 pills with a placebo pill; and the final group is taking two placebo pills. Manson explains that the trial has a cost-effective design that allows the investigators to study two separate nutrients efficiently and look at their effects both independently and in combination.
The aim of the VITAL study is to see if taking daily dietary supplements of vitamin D3 or omega-3 fatty acids reduces the risk for developing cancer, heart disease and stroke in people who do not have a prior history of these illnesses. Manson says that VITAL has placed special emphasis on recruiting black participants and has enrolled 5,108, which is 20 percent of the study population. “We’re very much interested in whether vitamin-D supplementation may narrow the gap between whites and blacks in terms of cardiovascular mortality, heart failure, prostate cancer, breast cancer mortality, stroke and diabetes,” she says. “Many of these outcomes have higher rates in blacks than whites.”
But until the study concludes in 2017, Manson says, “The jury is still out on the benefits and risks of high-dose vitamin-D supplementation for nonskeletal outcomes.”

Not done with D
Many of the observations of vitamin D affecting the cardiovascular, muscle and liver hepatic systems may be indirect effects, points out Pike. “Vitamin D has a pervasive effect on the maintenance of calcium and phosphorus levels in the blood,” he says. When systems go awry in the presence of the vitamin-D deficiency, it is not clear whether the organs are experiencing a direct effect of the deficiency or an indirect effect through the disruption of mineral metabolism brought on by the vitamin-D deficiency.
Experts say that the controversy over vitamin D also highlights the need to rethink using the prohormone 25-hydroxyvitamin D as a measure of the body’s overall vitamin-D status. We measure 25-hydroxyvitamin D because it’s blood-borne and stable over several days. But just because it’s easy to measure doesn’t mean it’s the right thing to measure. Adams, Hollis and others say that the standard serum measurement is a surrogate measure: It doesn’t show how much of the prohormone is free of the binding protein and available to be turned into the active hormone. This is important, says Adams, because some isoforms of the serum vitamin D-binding protein bind more avidly to 25-hydroxyvitamin D. These isoforms are known to be expressed specifically in blacks, once again giving a misleading interpretation of their overall vitamin-D levels.
Questions also persist about the vitamin-D receptor, which are as simple as “Where is it found?” Some experts, like Plotnikoff, say that vitamin D’s far-reaching effects in the body make sense because the receptor is found in every tissue. But others disagree. “Some of us are not convinced that significant levels of vitamin-D receptors are routinely expressed in many of those cells and tissues” in the cardiovascular and muscle systems, says Pike. “Try as we might, but over literally 30 years we have never been able to show vitamin-D receptors present in gross muscle tissue.”
Pike says some claims have been made in the literature about finding the vitamin-D receptor in all kinds of tissues but the data are generally weak. In those cases, investigators studying skeletal muscle, as an example, “grind up tissue, let cells grow in culture and then measure the vitamin-D receptor. Sure enough, there it is,” explains Pike. “The reality is growing those cells causes them to differentiate and change. Smooth muscle cells are notoriously able to differentiate into other cell types. The presence of receptor in those cell lines just doesn’t cut it. It’s just not right.”
Plotnikoff, Hollis and others who think we should be taking in higher doses of vitamin D are frustrated. They believe that scientific and health authorities have paid no heed to their warnings. Plotnikoff says it’s heartbreaking to see patients, like the woman he took care of, suffer. “People are miserable. They are put on all kinds of medications and misdiagnosed with metastatic breast cancer or depression or something else,” he says. “Vitamin D is cheap and easy.”
But observations like this are not yet backed up by large-scale studies, says Pike, and lead to problems: “Clinicians see one patient that happens to take a vitamin D pill and the next day, they get over the flu. Vitamin D treats the flu! This is nonsense.”
The need for more research is a unifying sentiment. Experts say that, despite vitamin D being discovered a century ago, research into it lapsed once rickets was cured. The field saw a resurgence once DeLuca and colleagues demonstrated in 1968 that vitamin D required activation inside the body to work as well as after the cloning of the vitamin-D receptor in the late 1980s. But fundamental gaps in understanding remain. For instance, researchers still don’t know the molecular details of how the vitamin-D receptor heterodimer complex works at regulatory sites to influence gene expression.
So when Plotnikoff says “It’s mindboggling that there isn’t more attention to be paid to vitamin D,” that’s a statement all vitamin-D experts can agree on.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles
CRISPR epigenome editor offers potential neurodevelopmental gene therapies
Scientists from the University of California, Berkeley, created a system to modify the methylation patterns in neurons. They presented their findings at ASBMB 2025.
Finding a symphony among complex molecules
MOSAIC scholar Stanna Dorn uses total synthesis to recreate rare bacterial natural products with potential therapeutic applications.

E-cigarettes drive irreversible lung damage via free radicals
E-cigarettes are often thought to be safer because they lack many of the carcinogens found in tobacco cigarettes. However, scientists recently found that exposure to e-cigarette vapor can cause severe, irreversible lung damage.

Using DNA barcodes to capture local biodiversity
Undergraduate at the University of California, Santa Barbara, leads citizen science initiative to engage the public in DNA barcoding to catalog local biodiversity, fostering community involvement in science.
Targeting Toxoplasma parasites and their protein accomplices
Researchers identify that a Toxoplasma gondii enzyme drives parasite's survival. Read more about this recent study from the Journal of Lipid Research.

Scavenger protein receptor aids the transport of lipoproteins
Scientists elucidated how two major splice variants of scavenger receptors affect cellular localization in endothelial cells. Read more about this recent study from the Journal of Lipid Research.

