MCP: Scott syndrome and the smallest sample size
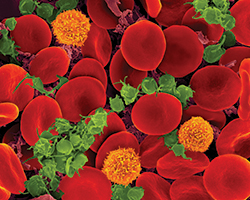
Scott syndrome is a dysfunction of blood platelets, which are the tiny circulating discs that initiate coagulation. It’s a rare bleeding disorder: There are only three known Scott syndrome patients worldwide. This dearth means that researchers must come up with ingenious ways to get the most data out of limited blood samples.
In a recent paper published in the journal Molecular & Cellular Proteomics, researchers have combined quantifications of the proteome, phosphoproteome and proteolytic cleavage sites to characterize platelet functions and modifications from blood samples from one patient. Of the three people worldwide with Scott syndrome, only one, who lives in the U.K., was available for blood donations when the researchers embarked on their study.
The disorder is homozygous recessive. Both copies of the inherited alleles that normally would code for anoctamin-6 are faulty in this patient.
Blood platelets lacking anoctamin-6, which is a channel protein for ions and phospholipids, are unable properly to localize the phospholipid phosphatidylserine, which normally stimulates the coagulation process. This dysfunction interferes with the platelets’ production of thrombin, which is needed to convert the parent molecule fibrinogen to the sticky fibrin strands that anchor blood clots.
While there is a diagnostic test for prothrombin consumption that can verify Scott syndrome’s thrombin-formation deficiency, this is not performed routinely, which may cause the disease to go undiagnosed.
The team of researchers, led by Johan P. Heemskerk at Maastricht University in the Netherlands and René P. Zahedi at the Leibniz Institute of Analytical Sciences in Germany, treated blood platelets from the Scott syndrome patient and from control blood donors with thrombin, ionomycin and a mixture of convulxin with thrombin. All of these compounds promote exposure to phosphatidylserine to some extent in control platelets but not in Scott syndrome platelets.
The researchers then extracted the proteins in the platelets that had been treated by the compounds and labeled them with isotopes. Then they fragmented the proteins into smaller peptides and used enrichment methods to purify the phosphopeptides and peptides that had been cleaved inside of the platelets.
This approach allowed the researchers to analyze simultaneously the proteome, phosphoproteome and N-terminome of each platelet sample. “You get a lot of information from a very small blood amount,” says Heemskerk.
The proteomic analysis confirmed the absence of anoctamin-6 in the Scott syndrome platelets as well as the upregulation of the water-channel protein aquaporin-1. The upregulation of aquaporin-1 may be a compensatory reaction for impaired ion and phosphatidylserine transfer.
By examining the peptides with phosphorus groups in each sample, the investigators saw strong similarities between Scott syndrome platelets and control platelets that both were treated with thrombin. As thrombin causes only mild exposure to phosphatidylserine, this finding indicated that many other activation processes in the patient’s platelets were unaffected.
The Scott syndrome platelets treated with ionomycin and the convulxin mixture, both of which cause high exposure to phosphatidylserine, showed an increase in the number of protein sites where phosphorus-containing groups were added.
However, the protease’s consensus motif wasn’t well-defined in research literature. The researchers were able to identify this motif and confirm that the Scott syndrome platelets showed a lower expression of calpain.
“I think it was the first time a study combined these three things to quantify the proteome, the phosphoproteome and the N-terminus protein from a blood sample using platelets that are from a patient, not from cell culture,” notes Zahedi.
The approach will allow the researchers to interrogate more fully limited samples from Scott syndrome patients to look for spliced genes that might be producing low levels of anoctamin-6. Zahedi and Heemskerk plan to continue their work by examining the genetic variation of anoctamin-6 across various individuals and compare it with altered activation levels of platelets and altered expression levels of the proteome.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

Using DNA barcodes to capture local biodiversity
Undergraduate at the University of California, Santa Barbara, leads citizen science initiative to engage the public in DNA barcoding to catalog local biodiversity, fostering community involvement in science.
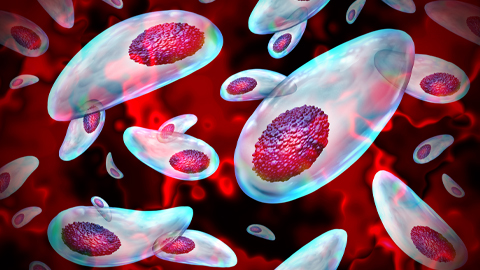
Targeting Toxoplasma parasites and their protein accomplices
Researchers identify that a Toxoplasma gondii enzyme drives parasite's survival. Read more about this recent study from the Journal of Lipid Research.

Scavenger protein receptor aids the transport of lipoproteins
Scientists elucidated how two major splice variants of scavenger receptors affect cellular localization in endothelial cells. Read more about this recent study from the Journal of Lipid Research.
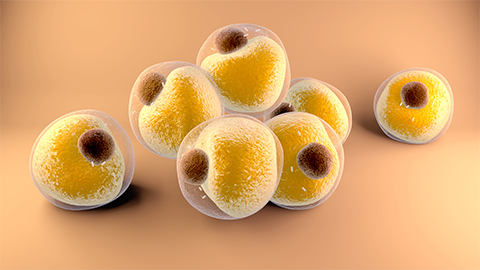
Fat cells are a culprit in osteoporosis
Scientists reveal that lipid transfer from bone marrow adipocytes to osteoblasts impairs bone formation by downregulating osteogenic proteins and inducing ferroptosis. Read more about this recent study from the Journal of Lipid Research.

Unraveling oncogenesis: What makes cancer tick?
Learn about the ASBMB 2025 symposium on oncogenic hubs: chromatin regulatory and transcriptional complexes in cancer.

Exploring lipid metabolism: A journey through time and innovation
Recent lipid metabolism research has unveiled critical insights into lipid–protein interactions, offering potential therapeutic targets for metabolic and neurodegenerative diseases. Check out the latest in lipid science at the ASBMB annual meeting.

