Shedding light on Usher syndrome
Sept. 16 marks Usher Syndrome Awareness Day, a designation that is far from arbitrary. The positioning of this observance near the fall equinox has a powerful intent: The ensuing days contain more darkness than light, poignant symbolism for those living with the varying levels of deaf–blindness that characterize Usher syndrome.
Despite being a relatively rare disease, affecting only around 400,000 people globally, Usher syndrome is the most common cause of genetic deaf–blindness. The disorder manifests in a few different sets of patterns but always impacts hearing and visual capabilities, often also causing balance issues stemming from vestibular dysfunction.
In recognition of the observance, ASBMB Today talked to two patients about the condition and how it affected their pursuit of education and training in the sciences.
Classifications
Usher syndrome is broadly divided into three clinical categories, which all adhere to different timelines.
- Type 1 describes the most immediate symptomatic manifestation, with individuals typically experiencing profound hearing loss from birth and signs of rapid vision decline within the first decade of life, in addition to vestibular issues that may delay normal walking benchmarks.
- Type 2 usually also includes congenital hearing loss but a more delayed progression of vision degeneration, with vision loss typically presenting within the second decade of life.
- As the least common form of Usher syndrome, Type 3 presents with normal hearing and visual capabilities and variable decline in these capacities, as well as vestibular function.
Meet Megan Lengel
Megan Lengel volunteers as a young adult coordinator for the Usher Syndrome Coalition, in addition to her job as an educational consultant for the nonprofit One Love Foundation.
Lengel was diagnosed with Type 1B of Usher syndrome around the age of seven, when deteriorating vision became a challenge in addition to her congenital deafness. Until receiving her cochlear implant at around age 2 and a half, Lengel communicated solely through American Sign Language.

Lengel graduated from the University of Mary Washington in 2019 with a degree in psychology and sociology. While some of her professors actively and enthusiastically developed different ways to help her learn throughout a class, Lengel dealt with other professors who were unwilling to wear a Phonak microphone that would transmit audio directly to her cochlear implant or who would be too busy or overwhelmed to provide captioning on videos.
She noted that her accessibility needs changed over time, as the vision loss associated with Usher syndrome is progressive. For example, she shared that she was much more able to use a microscope in high school than in college.
Before college, Lengel attended schools with prominent deaf programs. When applying to colleges, she focused on schools that had disability services offices with staff dedicated to offering personalized assistance, an asset that she said most colleges don’t have.
Lengel said her approach to asking for accommodations was based on a framework of assessing what was realistic for her instructors to provide, a responsibility that she feels many children with disabilities are taught to deal with early on.
“Self-advocacy was something that was really pushed into us as kids,” Lengel said. “There's this narrative of ‘We have to teach these kids independence. We have to teach them to not rely on other people too much because nobody is going to give them what they need.’”
“I would cooperate too much, basically,” she continued. “I would internally say, ‘OK, I need this, but they’re not gonna be able to give me this, so how can I ask for what I know they’ll give me?’ That was a very conscious thought.”
Lengel added that her relationship to self-advocacy has grown healthier since leaving school, sharing that she found many people willing to provide accommodations once she expressed her needs more clearly.

The science of the syndrome
Usher syndrome is autosomal recessive, meaning both parents must pass down a mutated gene.
Researchers have pinned down at least nine crucial genes so far, including a current list of MYO7A, USH1C, CDH23, PCDH15, USH1G (SANS), USH2A, ADGRV1, WHRN and CLRN1, that are all linked to the hearing and vision issues associated with Usher syndrome.
These genes encode a variety of proteins, coined USH proteins, that are expressed in the sensory cells of the auditory system, hair cells and the sensory cells of the visual system, photoreceptors.
USH proteins carry out an array of functions, including adhesion, signaling, scaffolding and transport. These proteins are found throughout hair cells and photoreceptors, but the dysfunction of USH proteins caused by Usher syndrome specifically disrupts the function of the sensory cilia regions of these cells.
In terms of auditory capabilities, many USH proteins are involved in the formation and structure of stereocilia, the ciliary protrusions from hair cells that are key to conveying signals from the ear to cortical areas. USH protein complexes play vital roles in the linkages between stereocilia, specifically in the delicate machinery of tip links perched at the ends of these stereocilia, a system that allows a hair cell to mechanically receive sound that it can then transcribe into signals to be sent on to the brain.
If essential proteins are rendered dysfunctional from mutations in USH genes, this whole process of sound transduction is blocked. Since hair cells are also an important feature of the vestibular system, mutations in USH genes can cause severe balance issues.
Photoreceptors in the retina also have ciliary structures, in which USH proteins have been identified. The cilia in photoreceptors, however, don’t follow the same organizational pattern of the stereocilia in the inner ear; researchers have yet to fully grasp exactly how USH protein complexes interact in these cilia and throughout the photoreceptor cell, although they are associated with membrane function and support.
The progressive vision loss associated with Usher syndrome is caused by retinitis pigmentosa, which describes a gradual loss of integrity and function of rods and, later, cones, the two types of photoreceptor cells present in the retina. The precise mechanism of this decay is not yet fully mapped out, but it is some combination of degenerated photoreceptors, retinal pigment epithelial cells and Müller glial cells.
Although the rate of retinal degeneration varies among clinical types of Usher syndrome and, on a more specific scale, among individuals, all cases began with the slow degeneration of rods. As rods are responsible for our ability to see in low light and around our periphery, this gradual loss manifests first as issues with contrasts and the presence of scotomas (small areas of blindness in our visual field), transitioning to major peripheral and night vision loss, then in most cases, eventually tunnel vision and legal blindness.
Recent research
Recent research includes potential insights into the structure of the USH protein complex key to maintaining links between stereocilia in hair cells. By studying a homolog complex, the inner microvillar adhesion complex that links microvilli in the intestine, researchers shed light on a component of the USH complex, the protein CALML4, that functions as a light chain for the myosin-7a base of the complex. This research suggests the gene associated with CALML4 as another potential causative gene for a subtype of USH1.
Additionally, there is recent evidence for a pattern between certain atypical forms of Usher syndrome, potentially underlying an Usher syndrome Type 4. These cases, linked by variants in the ARSG gene, generally display a shared phenotype of late-onset retinitis pigmentosa, involving a ring scotoma and progressive hearing loss. Further research is necessary to unequivocally confirm an addition to the clinical forms of Usher syndrome.
Diagnosis and treatment
Currently, no cure exists for Usher syndrome. Successful treatment and support are bolstered by catching the disease early, which is accomplished through neonatal screening and genetic tests.
Retinitis pigmentosa can be diagnosed through eye exams and electroretinography.
Babies diagnosed with congenital deafness may benefit from assistive hearing devices, cochlear implants and/or American Sign Language.
Other methods of managing symptoms include balance strengthening exercises, orientation and mobility training and exposure to and/or instruction in braille, depending on where the individual is in their journey. Individuals may also choose to use tactile sign.
Meet Monica Pruitt
While Usher syndrome can complicate many of the tasks of daily life, it can be an extra hurdle in the realm of science.

With hearing impairments but seemingly functional vision for much of her life, Monica Pruitt wasn’t diagnosed with Usher syndrome Type 2A until she was 29. She said she felt lucky that she encountered a doctor who was able to connect her hearing and vision loss to the rare pattern of Usher syndrome.
“I didn't know I was going blind. I didn't know I had Usher syndrome. I was just at the eye doctor for a routine checkup,” Pruitt shared. “My eye doctor started … testing my peripheral vision and I couldn't see his hand unless his fingers were right in front of his face!”
Pruitt’s late diagnosis meant that she experienced a different set of struggles than individuals diagnosed at birth. While she didn’t face the stigma associated with a rare genetic disease, Pruitt had to learn to subtly advocate for herself, without understanding why she had certain needs. She rationalized her failing eyesight by writing her coping mechanisms off as personality quirks, including not venturing outside after dark for much of her 20s, a trend that continued as her night vision worsened.
“I was strictly a daylight person, but I never thought anything of it, I never attributed it to anything,” Pruitt said. “When I was going on my interviews for my first real science lab, one of my criteria was if the lab wasn’t well lit, I wouldn't even consider it, and so now obviously it makes sense why that would be so important to me.”
As an undergraduate at the University of Maryland, Baltimore County, Pruitt studied biochemistry and molecular biology and was the campus’s American Chemical Society student chapter president. She also worked in a lab at Johns Hopkins University for nearly two years.

Pruitt said she enjoyed lab work immensely, noting that many of the strategies she unknowingly used to make lab work more accessible translated into skills that are valuable in the scientific world.
“In the labs, I was always … the more neurotic one, and everything had its place, and everything had a home, and I like things to be very neat,” Pruitt said, describing how she kept her lab station highly organized. “Now I realize it’s because it's hard, when it's messy, to find things.”
In interviews for lab positions, she said, “I could say things like ‘I pay attention to detail,’ and that’s something admired in the scientific community,” she continued. “There's a kind of metaphorical and literal tunnel vision that comes with the condition; that’s something that’s admired in science.”
In terms of accommodations in laboratories and science spaces, Pruitt notes the availability of tools such as the Roger Pen, a wireless hearing device that can be placed on a lab bench to transmit conversations around the room, and adaptations for microscopes that render a larger, high-contrast image, or include an automated cell counter.
Pruitt said that often the greatest obstacle to accessibility is the understanding of other people. She shared how she’ll use her cane in part as a reminder to other people that she has impaired vision and hearing.
Pruitt, who is now a communications assistant for the Usher Syndrome Coalition, offered a direct message to readers:
“Usher syndrome research has come a long way, but there is still so much more work to be done, especially on a biochemical and molecular biology level,” she said. “To the reader of this magazine: If they're looking for a research project for anything having to do with cilia or M3 neurons or calcium channel ions, (Usher syndrome) is a systematic and interdisciplinary condition that warrants attention from all facets of science.”
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles
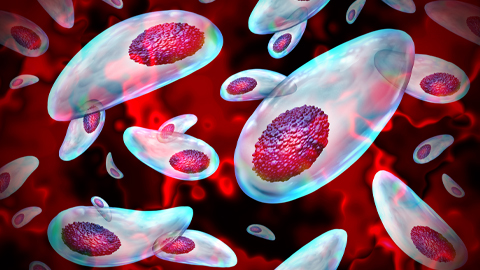
Targeting Toxoplasma parasites and their protein accomplices
Researchers identify that a Toxoplasma gondii enzyme drives parasite's survival. Read more about this recent study from the Journal of Lipid Research.

Scavenger protein receptor aids the transport of lipoproteins
Scientists elucidated how two major splice variants of scavenger receptors affect cellular localization in endothelial cells. Read more about this recent study from the Journal of Lipid Research.
Fat cells are a culprit in osteoporosis
Scientists reveal that lipid transfer from bone marrow adipocytes to osteoblasts impairs bone formation by downregulating osteogenic proteins and inducing ferroptosis. Read more about this recent study from the Journal of Lipid Research.

Unraveling oncogenesis: What makes cancer tick?
Learn about the ASBMB 2025 symposium on oncogenic hubs: chromatin regulatory and transcriptional complexes in cancer.

Exploring lipid metabolism: A journey through time and innovation
Recent lipid metabolism research has unveiled critical insights into lipid–protein interactions, offering potential therapeutic targets for metabolic and neurodegenerative diseases. Check out the latest in lipid science at the ASBMB annual meeting.

Melissa Moore to speak at ASBMB 2025
Richard Silverman and Melissa Moore are the featured speakers at the ASBMB annual meeting to be held April 12-15 in Chicago.

