Researchers unravel mysteries of puzzling bacterial signals in our blood
A type of bacteria that live in our mouths and guts send signals — in the form of lipids — through our blood, which could be good or bad, depending on the context. A multidisciplinary collaboration of University of Connecticut researchersis pioneering the study of these bacterial signals and the surprising roles they play in the human body.
They’re in your mouth
Porphyromonas gingivalis is a pathogenic bacterium in the phylum Bacteroidota (formerly Bacteroidetes). It causes a destructive form of periodontal disease called periodontitis.
Dr. Frank Nichols, professor of periodontology in the UConn School of Dental Medicine, became interested in Porphyromonas gingivalis in the early 1990s and has been fascinated, and surprised, by the pathogen ever since.
Nichols explains that P. gingivalis colonizes the spaces between teeth and gums, and, in the absence of brushing and flossing, over time the environment and community gradually changes from healthy to pathogenic. The bacteria build up in plaque, and, as the bacteria grow and die, they release lipids from their cell walls, which the immune system recognizes as signals of infection, triggering inflammation. Over time, the inflammation becomes chronic and can result in tissue damage and tooth or bone loss.
Nichols wanted to know more about bacterial lipid triggers, so he started extracting and characterizing them. Initially he was examining lipopolysaccharide, a common cell wall product produced by all gram-negative organisms.
“When LPS is expressed on the surface of the cells in the gut, it helps to protect the organisms from the bile salts, dissolution and destruction processes,” Nichols says. “But we don’t have bile in our mouths, so there’s no reason for these bugs to have this LPS.”
In addition to the puzzle of why mouth bacteria would have gut-protective lipids in their cell walls, Nichols soon found another: In periodontitis-diseased tissues, P. gingivalis was present, but not much LPS was evident in tissues. At first, he didn’t believe this result, but after reproducing the experiment he noticed a distinction.
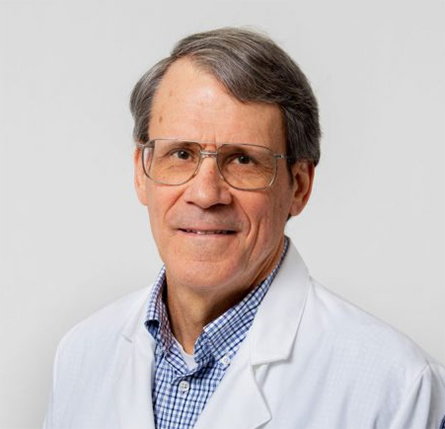
School of Dental Medicine.
“There is not so much LPS in the tissues, but there are a lot of other kinds of bizarre lipids from P. gingivalis,” says Nichols. “I knew this because a unique fatty acid identified the presence of these lipids. These lipids are unique to the Bacteroidota, the phylum P. gingivalis belongs to. Periodontal disease is not like having a microbial infection around the teeth where the organisms invade the tissues and cause abscess formation, swelling, pain. Instead, periodontal disease elicits a chronic inflammatory response by the host.”
How the organisms elicit this chronic inflammatory process is thought to involve the release of virulence factors, such as LPS, which are then taken up by immune cells, or through simple diffusion processes where the bacterial lipids passively slip into the host’s cells. Physical properties of lipids facilitate diffusion and can help them move around quite a bit, a quality that Nichols’ work would highlight.
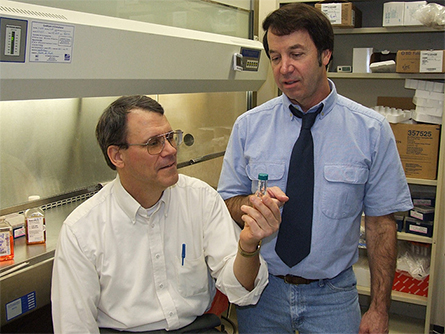
Nichols continued extracting and trying to learn more about the lipids and their travel habits. He started collaborating with UConn's Michael Smith over the course of the next 20 years.
“He had terrific graduate students that were synthesizing these lipids and verifying the structures,” Nichols says. “It was a terrific collaboration, and we were able to confirm those structures in part because of that synthetic work that was done in his lab.”
Extracting and characterizing these lipids is highly specialized work, Nichols explains, and the collaboration helped build a collection of lipids that he has since shared with other researchers.
Nichols subsequently found that these lipids accumulate more extensively when there’s significant disease, like destructive periodontitis. The results, though significant, were met with skepticism, says Nichols, as some others in the field refused to believe it could be anything other than LPS he was measuring.
Nichols didn’t give up then, and has continued growing the bacteria, extracting the lipids, and screening their biological activity — and this has led to even more collaborations.
They’re sending signals through your blood
Dr. Robert Clark’s interest was piqued as he followed Nichols’ progress in studying these lipids.
Clark, a professor at UConn School of Medicine's immunology department, is interested in autoimmune diseases, such as multiple sclerosis, and in the early 2000s, he says, the microbiome was a very hot topic — with thousands of publications coming out studying relationships between the microbiome and diseases but little work on exactly how the bacteria were potentially mediating things. He says Nichols was wise enough to look deeper by examining what the bacteria make in terms of lipids.
Clark also was struck by the fact that Nichols had shown the lipids are distinct to Bacteroidota, which are found not only in the mouth but also in the GI tract. They consitute 30% to 50% of the organisms found in the GI tract microbiome.
Clark says he and Nichols would talk about their work when running into each other on elevators or in passing: “We knew each other and would share results. One day, I asked if he thought these lipids that were produced by bacteria in the mouth and GI tract were affecting systemic human health.”
That elevator conversation launched their collaboration. Clark proposed they see if these bacterial lipids are present in the bloodstream. In 2013, they published work showing they accumulate in structures in blood vessels that can lead to thickening or blockages called atheromas.
“Every person has these lipids in their blood. That was surprising, because that’s a bacterial product, and it can’t be confused with something we make. It’s totally different,” says Clark. “You, sitting there, have bacterial products floating around in your bloodstream that are doing things to you.”
Next, Clark wanted to see what the lipid levels were like in the blood of MS patients, and they found that the bacterial lipid levels were lower in MS patients, a very surprising result. They expected, if anything, that patients with the autoimmune disease would have more lipid present.
“There are two phases of our immune system,” Clark says. “One is the adaptive immune system with T and B cells, but there is also the innate immune system, which gets the ball rolling in any immune response. These bacterial lipids are stimulants for the innate immune system, and it is thought that people with autoimmune diseases have overreactive immune systems that attack self-tissue in general. We realized there is something strange happening here.”
The fact that these stimulatory lipids were present in lower levels in MS patients revealed a new level of complexity that Clark has been since working to understand.
They’re in your gut
The mystery also caught the attention of Christopher Blesso, associate professor in the College of Agriculture, Health and Natural Resources' nutritional sciences department.
“I first came into contact with Nichols by reading a UConn Today article,” Blesso says. “I reached out to him because I was interested in figuring out if the diet affected these bacterial lipids.”
Blesso studies dietary fats and had never considered bacteria as a possible or significant source of lipids. Nichols was happy to collaborate, and it culminated in Blesso’s recent publication in the Journal of Lipid Research — another breakthrough in deciphering the roles of these lipids.
Blesso was interested in looking at different diets and their impacts on the gut microbiome.
“A lot of the initial studies with obesity and unhealthy diets, like high-fat diets, showed Bacteroidota were suppressed in those high-fat conditions,” Blesso says. “Once the individual lost weight or started eating a higher fiber diet, the Bacteroidota population would tend to go back up again.”
Blesso reasoned that high-fat diets lead to a decrease of Bacteroidota and that would lead to changes in the lipids produced.
For the experiment, they fed mice who are genetically predisposed to high cholesterol a diet that mimics a high-fat, Western diet to induce atherosclerosis and liver inflammation. Another group of mice serving as a healthy reference were fed a regular, low-fat, plant-based diet called a chow diet.
They then administered one of the bacterial lipids called L654 to the mice to mimic chronic inflammation, with an initial hypothesis that these conditions would speed the development of atherosclerosis and liver inflammation in the Western diet group.
Again, the lipids surprised the researchers.
“We assumed that if we’re exposing the animals to these lipids that we would see more inflammation and atherosclerosis. We actually found the opposite,” says Blesso.
In the case of the high-fat, Western diet-fed group, the lipid lowered the inflammation of the liver and liver injury markers, and, overall, seemingly had an immunosuppressive effect that protected the mice from atherosclerosis development, says Blesso. However, the biggest effects they saw were in the liver.
“To me, it’s more interesting when you don’t find what you thought you’re going to find,” Blesso says. “It unlocks new questions.”
Blesso suspects the lipids act almost like a brake for the immune cells in the liver.
“I’m hypothesizing that these bacterial lipids are signals that help form a tolerance, and, if you lose the signal because of a high-fat diet or obesity, that will actually promote a breakage of that tolerance, and the immune system will start to attack the liver,” he says. “Without that tolerance, you have liver inflammation and liver disease. It seems like the high-fat diet and obesity break that tolerance, and this leads to liver inflammation.”
While the researchers are still not entirely sure how the lipids make their way into the bloodstream, it is clear they can have big impacts on physiological processes.
Blesso’s findings echoed Clark’s work by showing that these lipids may not be all that bad and that their impact on the body is context-dependent.
A Goldilocks situation
The researchers, bolstered by unexpected and exciting results, are pressing on and continue to enjoy the collaboration, across disciplines and campuses.
“We are just trying to figure out what’s going on together. Developing the methods to figure out how to measure these lipids takes a lot of people,” says Blesso.
Another collaboration that makes this work possible is with Anthony Provatas, assistant research professor in the chemistry department and a researcher in the Organics Environmental Analytical Laboratory at the Center for Environmental Sciences and Engineering, who helps analyze and characterize the samples.
Blesso says, “We’re going to keep working together into the future and will hopefully figure out how they’re absorbed and transported and how they affect different disease states.”
These latest findings give Clark new hope for understanding the lipid role in MS: “Now we show two cases where the lipids are lower, and this is somehow regulating or dysregulating the immune system, making it stronger.”
The results connecting the microbiome with diet and systemic inflammation led to the question of whether antibiotics could further influence the lipid producers. On this, he says, stay tuned, but he suspects there may be a sort of “Goldilocks phenomenon” at play where too much or too little lipid could result in hyperactivity in the immune system.
“It’s a unique system to study,” Clark says. “Most researchers don’t believe us. Scientists don’t like to leave their comfort zone. There are probably 100 papers that say slightly different things about which bacteria are changing when you have this disease, but no one is connecting the dots for how that might work.”
Clark points out that many different Bacteroidota produce these lipids, so studies purely looking at changes in the microbiome will not be as telling as studies which look more closely at the roles those bacteria play.
“These lipids are among the very few molecules that anyone’s identified. For instance, you could lose bacteria X, but if bacteria Y is still there, there may be no effect if they both make the same lipid. Whereas you could have bacteria Z gain in numbers and have a major change because the lipid they’re producing is different. No one else is measuring these, and that is good and bad. Good in that our group is pioneering this field but bad because reviewers, if they’re not doing this work, they tend to say ‘No way. This couldn’t be,’” says Clark.
Nichols adds that, for this reason, the field remains wide open: “People don’t work on lipids for the most part, because they are tough to work with, but it’s what I’ve been working on for 25 years. I’m not going to give up.”
This work is catching the attention of other researchers, and Nichols’ collection of lipids is fueling that research. For instance, one scientist is looking at genes involved in the synthesis of the lipids and another is looking at potential connections with Alzheimer’s.
There is more to these lipids and the bacteria that produce them, and the collaborators are determined to keep working to understand. As Nichols says, “It’s all because of this one bug” and a refusal to listen to the naysayers.
This article was republished with permission from UConn Today. Read the original.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles
Finding a symphony among complex molecules
MOSAIC scholar Stanna Dorn uses total synthesis to recreate rare bacterial natural products with potential therapeutic applications.

E-cigarettes drive irreversible lung damage via free radicals
E-cigarettes are often thought to be safer because they lack many of the carcinogens found in tobacco cigarettes. However, scientists recently found that exposure to e-cigarette vapor can cause severe, irreversible lung damage.

Using DNA barcodes to capture local biodiversity
Undergraduate at the University of California, Santa Barbara, leads citizen science initiative to engage the public in DNA barcoding to catalog local biodiversity, fostering community involvement in science.

Targeting Toxoplasma parasites and their protein accomplices
Researchers identify that a Toxoplasma gondii enzyme drives parasite's survival. Read more about this recent study from the Journal of Lipid Research.

Scavenger protein receptor aids the transport of lipoproteins
Scientists elucidated how two major splice variants of scavenger receptors affect cellular localization in endothelial cells. Read more about this recent study from the Journal of Lipid Research.

Fat cells are a culprit in osteoporosis
Scientists reveal that lipid transfer from bone marrow adipocytes to osteoblasts impairs bone formation by downregulating osteogenic proteins and inducing ferroptosis. Read more about this recent study from the Journal of Lipid Research.

