JBC: The mystery of metformin
Jean Sterne discovered in 1959 that metformin, or dimethylbiguanide, lowers blood glucose levels in people with Type 2 diabetes. Researchers now are studying metformin as a therapeutic agent for managing such maladies as fatty liver disease, cardiovascular disorders and cancer. Yet while the mode of action for other drugs — including the anticancer agent Taxol, the analgesic aspirin and the antidepressant Prozac — is well understood, metformin’s exact molecular mechanism remains a mystery.
 Metformin is prescribed to control Type 2 diabetes, but the drug’s exact molecular mechanism remains a mystery.Wikimedia Commons
Metformin is prescribed to control Type 2 diabetes, but the drug’s exact molecular mechanism remains a mystery.Wikimedia Commons
This is not for lack of trying. The journey to discover how metformin works includes two seminal studies published in the Journal of Biological Chemistry, now recognized as JBC Classics.
Mohamad-Yehia El-Mir and colleagues reported in 2000 that metformin inhibits respiratory complex I in the mitochondria of liver cells, or hepatocytes. This suggested that the authors had hit the bullseye of metformin’s molecular target. However, there was a wrinkle.
“Metformin’s effects on complex I were indirect,” said Eric Fontaine, one of the researchers involved in this work and now at Université Grenoble Alpes in France. This indirect effect decreased cellular respiration and was highly specific, solely affecting mitochondrial complex I — but only in intact hepatocytes.
“If we put metformin into isolated mitochondria, we did not observe an inhibition of complex I,” Fontaine said. The reason for this finding remains unclear, but metformin’s indirect effect has been reproduced by the authors of the El-Mir paper and by other labs.
Later studies have reported that metformin directly inhibits complex I in isolated mitochondria, Fontaine said, but only in state 3 of complex I, when ATP is produced, a state that the El-Mir study did not examine. However, the metformin concentrations required to affect complex I activity directly are consistently higher than those yielding the indirect effect, suggesting the two effects are not linked. Confusion about metformin’s effect on complex I persists in the literature and likely will be resolved only after metformin’s molecular target is pinpointed.
Another clue to metformin’s cellular target came to light in a 2001 paper reporting that metformin activates AMP-activated protein kinase, or AMPK. Gaochao Zhou and colleagues observed that metformin-induced AMPK activation suppresses glucose production in the liver through gluconeogenesis and also promotes glucose uptake into skeletal muscle. The study represented an important advance, according to David Carling, senior author of the second JBC Classics paper, which was published in 2002. However, “it wasn’t clear how metformin was causing AMPK to be activated, what the molecular mechanisms were,” he said.
This provided an opportunity for Carling’s lab, which had a long track record of studying AMPK.
Metformin’s effect on AMPK intrigued Carling because “AMPK acts as a very important, perhaps the most important energy sensor, within mammalian cells,” he said.
Having previously developed a skeletal muscle cell line called H-2Kb that provided a reliable model to study AMPK in muscle cells, Carling and his group were ideally positioned to take the next steps to look at AMPK’s role in mediating metformin’s effects.
“The first thing was that we got really good (AMPK) activation in this cell line, so that was brilliant,” he said. “We were able to confirm and reproduce that metformin really did give a very robust activation of AMPK.”
This was no small feat; metformin fails to get into cells that lack a specific transporter, organic cation transporter 1, or OCT1, a technical detail that wasn’t common knowledge at the time and may still bedevil research into metformin’s effects in cells. What’s more, the H-2Kb cells, unlike some commonly used cell lines, express high levels of an upstream kinase — liver kinase B1, or LKB1 — that phosphorylates and activates AMPK.
“The hindsight is that (the cells) were able to take up metformin,” Carling said, “and they expressed the upstream kinase that is required for activation of AMPK in response to metformin.”
With all these then-unknown factors in alignment, Carling’s research team set out to test whether metformin and another antidiabetic drug, rosiglitazone, activate AMPK by increasing the AMP-to-ATP ratio, a well-known AMPK inducer. The authors first demonstrated that rosiglitazone activates AMPK, a finding not previously reported, and that it does so by dramatically increasing the AMP-to-ATP ratio. However, metformin apparently did not measurably change the ratio. This finding prompted the authors to conclude that rosiglitazone and metformin activate AMPK via distinct routes.
But there was a hitch to that conclusion — with refinements in analytical methods, additional studies have shown that AMPK is sensitive even to very small changes in the AMP-to-ATP ratio. So small, in fact, that Carling and his team had been unable to see them.
“We didn’t have sensitive enough methods available for detecting very small changes in AMP,” Carling said.
So, although metformin is much less potent than rosiglitazone in increasing the AMP–to–ATP ratio, both appear to activate AMPK through the same general mechanism. “It’s been an interesting journey for the AMPK field to realize that the levels of change in the nucleotides that you need are incredibly subtle,” Carling said.
In an ironic twist, later studies have shown that AMPK is, in fact, activated via two routes: one through AMP-to-ATP ratio-stimulated phosphorylation by the upstream kinase LKB1 and another via calcium-induced phosphorylation by another enzyme, calcium/calmodulin-dependent kinase kinase 2, or CAMKK2.
“It turns out there are two distinct pathways, just not the ones that we thought,” Carling said.
Both Carling’s work on AMPK and that of El-Mir and colleagues on complex I show that metformin profoundly alters cellular energetics. “I think there are a lot of knock-on effects that interfere with complex I,” Carling said.
This might explain why it’s been so hard to pin down metformin’s direct target, but metformin’s elusive activity in the lab, its relatively weak effects on the AMP-to-ATP ratio and its impaired uptake into some cells might be why it continues to be an efficient and well-tolerated antidiabetic drug.
“The fact that it is a fairly poor drug turns out to be its strength — it’s very unusual,” Carling said. “I think metformin is a great example of why you shouldn’t get too hung up with mechanism (when you start) to test whether a drug is effective.”
This hasn’t stopped scientists’ search for metformin’s direct target in hopes of unraveling how it exerts its effects and improving on those effects to more efficiently manage diabetes or cancers that have emerged as potential targets of metformin-based therapies. Recent advances such as cryo-EM have enabled detailed structural studies of larger protein complexes, including complex I.
Carling believes researchers are much closer to finding out whether or how metformin interacts with complex I or other cellular structures. “(Complex I) is an obvious one to do,” he said.
Perhaps the long journey to solving the mystery of metformin’s direct target will soon come to an end.
Three of the scientists who made major contributions to these findings have since died: Mohamad-Yehia El-Mir and Xavier Leverve, first and senior authors, respectively, of the El-Mir et al. paper, and Lee Fryer, first author of the Carling group study.
Fontaine worked closely with El-Mir for about two years and remembers him as a great friend and colleague. And Leverve, he said, was an inspiring mentor. “He was a fantastic man — very, very charismatic. Everybody who met him wanted to work with him.”
Leverve’s training and experience as a physician in an intensive care unit may have spurred his interest in bioenergetics, leading him to study complex I and the compounds acting on it. “He had a very open mind from the clinic, especially in the ICU, where there is a kind of an energy failure during a septic shock,” Fontaine said.
Carling said he appreciates that his lab’s work has been nominated as a JBC Classic, but he also noted, “It’s a great shame that Lee is not around to see this recognition. Lee was a very productive scientist and had a big impact on my lab.”
This article has been edited for ASBMB Today. Click to read more JBC Classics.
 Martin J. Spiering is the technical editor at the Journal of Biological Chemistry. Follow him on Twitter.
Martin J. Spiering is the technical editor at the Journal of Biological Chemistry. Follow him on Twitter.Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

E-cigarettes drive irreversible lung damage via free radicals
E-cigarettes are often thought to be safer because they lack many of the carcinogens found in tobacco cigarettes. However, scientists recently found that exposure to e-cigarette vapor can cause severe, irreversible lung damage.

Using DNA barcodes to capture local biodiversity
Undergraduate at the University of California, Santa Barbara, leads citizen science initiative to engage the public in DNA barcoding to catalog local biodiversity, fostering community involvement in science.
Targeting Toxoplasma parasites and their protein accomplices
Researchers identify that a Toxoplasma gondii enzyme drives parasite's survival. Read more about this recent study from the Journal of Lipid Research.

Scavenger protein receptor aids the transport of lipoproteins
Scientists elucidated how two major splice variants of scavenger receptors affect cellular localization in endothelial cells. Read more about this recent study from the Journal of Lipid Research.
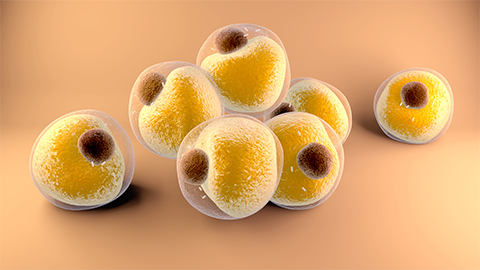
Fat cells are a culprit in osteoporosis
Scientists reveal that lipid transfer from bone marrow adipocytes to osteoblasts impairs bone formation by downregulating osteogenic proteins and inducing ferroptosis. Read more about this recent study from the Journal of Lipid Research.

Unraveling oncogenesis: What makes cancer tick?
Learn about the ASBMB 2025 symposium on oncogenic hubs: chromatin regulatory and transcriptional complexes in cancer.

