Myalgic encephalomyelitis
Lizzie Mooney is 12 years old. She is tall for her age with long blond hair. She likes to wear Chicago Bears pajama bottoms and a hoodie. She’s funny, making up games and teasing her siblings.
Lizzie excels in reading and math. She spends time crafting and watches science shows with her parents at night. But it’s hard for her to make it downstairs to the TV room. She can’t go to school. In fact, she might only leave her house once a week.
For the past three years, Lizzie has been sick.
The government estimates that as many as 1 million to 2.5 million Americans have the same disease as Lizzie: myalgic encephalomyelitis, or ME. Despite these numbers, you probably haven’t heard of ME. What you might have heard of instead is chronic fatigue syndrome, or CFS. This euphemism for ME conjures an image of someone who just doesn’t feel like getting out of bed.

her house or even eat meals at the table with her family.
For many ME patients, getting out of bed would be the highlight of their week or month. About 25 percent of patients are housebound, in rooms with the blinds drawn and noises muffled. Patients’ bodies are sensitive to all kinds of stimulation; they suffer from gastrointestinal problems, inability to sleep, chronic pain and the disease’s trademarks: cognitive dysfunction and post-exertional malaise, or PEM. Many patients describe PEM as a crash. Something as simple as a short walk can severely worsen a patient’s symptoms, leaving them bedridden, unable to recover, for weeks or months. There’s no telling how long the crash will last. Imagine having to decide between taking a shower and making yourself lunch. It could be your only activity for the week. Patients with ME have reported lower quality-of-life scores than patients with terminal cancer and heart disease.
Yet federal funding for ME research remains at a fraction of what is spent on each of these. In fact, research funding for ME remains less than what the government spends on headaches or hay fever. Multiple sclerosis funding is 12 times the funding for ME, but an estimated 400,000 patients in the U.S. have MS, fewer than half the number who have ME even according to the most conservative estimate.
When Lizzie got sick, her mother, Amy Mooney, took her to their primary care physician, who diagnosed Lizzie with a mononucleosislike illness. Lizzie spent the next four months in bed. Mooney took her to infectious disease doctors, rheumatologists, neurologists and gastroenterologists, but no one could make a diagnosis.
“The most painful moment was when an infectious disease doctor took me into the hallway,” Amy Mooney said. “He said, ‘Congratulations. Her blood work is completely normal. Nothing is wrong with her.’ In the patient room, they were asking Lizzie if we have a healthy family life: Do we have abusive family situations?
Are we going through a divorce?
“The physician at the pediatric hospital wrote a note to the school saying it was safe for her to go to school,” Mooney said. “‘Get her back to school. Kids with cancer go to school.’”
Lizzie hasn’t been to school since she was nine. She works at home with a private tutor when she can.

she retreats to her dark bedroom, where she sometimes shakes in pain for hours.
For decades, the search for pathogenic underpinnings for ME came up empty, and the disease was attributed to psychological causes. Stigma, skepticism and limited funding have fueled what advocates characterize as a vicious cycle that’s left a big hole in ME research. But advances in our understanding of the gut microbiome, cell-mediated immunity, mitochondrial dysfunction and dozens of other variables may open the door to new approaches to understanding and treating the disease.
While ME’s existence is no longer controversial, within the ME community, federal funding for ME research is. In recent years, the National Institutes of Health has spent between $5 million and $8 million a year on ME research. In 2017, the NIH earmarked $7 million for a first-time ME research collaboration of four centers. But some advocates say the government should be dedicating more than 50 times that amount.
Steps in the right direction?
Among those advocates is journalist Hillary Johnson, who says billions of dollars would be an appropriate figure.
Johnson spent almost a decade during the 1980s and 1990s researching the befuddling lack of interest in ME by government entities such as the Centers for Disease Control and Prevention and the NIH. She compiled her findings into a book, “Osler’s Web.”
In her book, Johnson chronicles the ’80s as a time when the CDC actively buried ME research and funding. She also casts Stephen Straus, a senior investigator in the Laboratory of Clinical Investigation at the NIH’s National Institute of Allergy and Infectious Diseases, or NIAID, from 1991 to 1999, as the chief villain. Straus published a number of studies on ME, some of which psychologized the disease. Straus went on to become the first director of the National Center for Complementary and Alternative Medicine. When he died in 2007, he was warmly remembered by his colleagues and was lauded by the NIH for what was then still called chronic fatigue research.

used for ME/CFS research.
Joseph Breen is the current chief of the immunoregulation section in the Division of Allergy, Immunology and Transplantation at the NIAID. “Fortunately, perspectives about the disease have changed,” Breen said. “Researchers now have the tools to explore possible etiologies of ME/CFS and future studies should be revealing, especially those with larger cohorts, initiated early after disease onset and with longitudinal follow-up.”
The NIH announcement in September of four grants totaling more than $7 million for fiscal year 2017, and continuing for the next five years, signifies a step in official ME recognition. The new NIH grants will support three collaborative research centers and a data-management coordinating center for ME research. One grant is going to researchers at Cornell University led by principal investigator and American Society for Biochemistry and Molecular Biology member Maureen Hanson. A 2016 study in Hanson’s lab found that ME patients’ microbiomes have significantly lower microbial diversity and a higher incidence of pro-inflammatory species than in healthy controls.
Hanson’s work also branches into fatty acid and lipid metabolism. Her lab produced a 2017 paper on a study that found significant disturbances in numerous fatty acid and amino acid metabolism pathways. Levels of energy-related metabolites, such as ATP and ADP, were significantly lower in ME patients. Acetylcarnosine and taurine, important to muscle tissues, also were less abundant.
Hanson and her colleagues at Cornell will use the new NIH grant to study post-exertional malaise using neuroimaging, metabolomics and single-cell RNA sequencing.
The researchers will take blood samples before and after the study participants ride stationary bicycles on two consecutive days.
To determine why ME patients usually can’t replicate their initial performances, the researchers will search their blood samples for biomarkers.
Hanson’s specific role in the project will be to study extracellular vesicles, which transport materials between cells. In healthy people, exercise induces release of these vesicles, which may mediate the beneficial effects of physical activity.
“This is going to be an important study to carry out — at the time we wrote our proposal, there were no published studies about extracellular vesicles in ME,” Hanson said.
If patients can fall into severe PEM after even basic activities, how could Hanson’s team find ME patients willing to do two days of exercise testing?

“Even though the exercise will likely induce a relapse, most of the patients don’t report that they never recover, otherwise we would never do it,” Hanson said of the tests. “In fact, some of these patients ask to return to obtain needed disability documentation. It is right now the most objective way for someone to demonstrate their disability. A lot of them have a great deal of trouble convincing insurance companies or the social security agency that they are actually disabled.”
U.S. medical record and insurance billing codes still classify ME as chronic fatigue — as a symptom rather than a disease. Even with a diagnosis, the insurance companies would not cover Lizzie’s prescription medications or supplements, which cost the Mooneys upward of $1,000 each month. One study estimates conservatively that ME patients pay $8,675 per year for treatments, and the direct cost to the U.S. healthcare system for all patients could top $7 billion.
An eight-decade mystery
Key moments in myalgic encephalomyelitis history
| 1934: | The earliest case of ME is observed and formally recorded as an outbreak of poliomyelitis among staff at the Los Angeles County General Hospital. |
| 1956: | The Lancet recommends the name “benign myalgic encephalomyelitis” to describe an outbreak in London; patients have neurological symptoms, myalgia and a number of other symptoms following an infection. |
| 1969: | The World Health Organization classifies the disease for the first time as “benign myalgic encephalomyelitis,” listing it as a neurological disorder. |
| 1970: | Two psychiatrists in the U.K. review reports of 15 outbreaks of patients with similar symptoms and deduce that the results are due to hysteria, as they see no physical signs of disease. |
| 1978: | An international symposium held at the Royal Society of Medicine drops the term “benign,” as it is not commensurate with symptoms reported by patients. |
| 1984: | Recorded instances are sporadic around the U.S. until the Los Angeles Times reports an outbreak on the shore of Lake Tahoe. Before the report, the Centers for Disease Control and Prevention sends two epidemiologists to investigate a severe flu-like illness with persistent symptoms. The epidemiologists return empty-handed just days later. |
| 1988: | The CDC names the disease now known as ME a “syndrome of chronic fatigue.” |
| 1989: | Two British studies attribute ME to a psychological disorder and a self-perpetuating lack of exercise, self-representing an investigative trend by psychological and psychiatric researchers. |
| 1990: | The CDC receives more than 2,000 calls per month from the public requesting information about a flu that never goes away, according to journalist Hillary Johnson. |
| 1991: | Researchers from the Wistar Institute in Philadelphia propose the retrovirus HTLV as a causative agent in a paper published in the Proceedings of the National Academy of Sciences. A blinded follow-up study by the CDC fails to replicate their results. |
| 1991: | The National Institutes of Health’s Stephen Straus publishes studies stating ME is a psychological disease and shares his findings at scientific talks and hospital grand rounds around the world. He refuses to comply with Freedom of Information Act requests by reporter Johnson to see his research data. He refuses to release information on how funding for disease research is spent. |
| 1996: | Hillary Johnson publishes her book, “Osler’s Web,” about a nine-year investigation into the ME/CFS research community. She alleges that research has been stifled and funds misused. |
| 1996: | Congress requests that the General Accounting Office and the Department of Health and Human Services investigate claims made in “Osler’s Web.” Both investigations verify the book’s contents. |
| 1999: | The ME/CFS Working Group is established at NIH. |
| 2009: | An article published in Science describes a link between murine leukemia virus XMRV and ME/CFS. The study cannot be replicated and is retracted in 2011. |
| 2011: | The PACE trial reports in The Lancet that cognitive-behavioral therapy and graded exercise therapy can benefit ME/CFS patients. Patients object to the methodology and results, organizing a petition and FOIA request for release of anonymized data. |
| 2015: | David Tuller publishes a lengthy methodological critique of the PACE trial. |
| 2016: | Independent analysis of data from the PACE trial by American biostatisticians in collaboration with patients fails to support the study’s conclusions. |
| 2016: | Advocates and patients organize across the country under the banner of #MillionsMissing to demand increased funding. Advocates and patients who are well enough to attend speak about how the disease has affected them, hang photos of homebound patients and set out pairs of shoes to represent patients who are too sick to join. Demonstrations expand to 25 cities worldwide in May 2017. |
| 2017: | The documentary film “ Unrest” is released, chronicling the life of its producer Jennifer Brea, an ME patient. |
| 2017: | The NIH announces it will award four grants totaling more than $7 million to establish centers for ME research. |
| 2018: | If high estimates of prevalence are accurate, up to 8 in every 1,000 Americans have ME. Hillary Johnson referred to ME in the 1980s and ’90s as an epidemic; she now calls the disease endemic. |

Also under the NIH grant, researchers led by Dikoma Shungu at Weill Cornell Medical College will do one of the first neuroimaging tests on ME patients experiencing PEM.The other two NIH research centers include a team at Columbia University that will look for microbial agents and evidence for immune responses to microbes and a team at the Jackson Laboratory in Farmington, Connecticut, that will study how the body’s immune system, microbiome and metabolism interact.
The Research Triangle Institute in North Carolina will house the data-management center, bringing data from the three centers into one database for standardization and providing tools for data processing and analytics.
“This is a very important step by the NIH,” Hanson said. “But we need more centers and individual studies relative to the burden of illness and number of people who are ill. The number of research dollars is really inadequate.”
Breen said he hopes that researchers will be encouraged by the NIH’s increased commitment to ME research and will continue to apply for more funds.
“The NIH ME/CFS working group functions as a team and we’re just starting the ME/CFS Collaborative Research Center program,” he said. “In the next five years, we hopefully will grow the community with a network of ME/CFS centers and small investigator-initiated research project grants.”
Millions missing

and she is a vocal advocate for increased
research funding. Here she speaks
as the host of a screening of “Unrest,”
a 2017 documentary about ME.
Rivka Solomon, 55, has had ME for 28 years.
When called for a phone interview, she didn’t answer, even though she had seemed eager to talk during email exchanges to schedule the interview. She called back 25 minutes late.
“Cognitively … I remembered your call, but then I forgot,” she said. “See, this is what happens. On bad days, my brain does not work well. And neither does my body. During a relapse it can take me 45 minutes to get up a set of stairs because I have to rest between each step.”
When Solomon was 21, she and her two roommates all got mononucleosis at the same time. Her friends got better. Solomon stayed sick for a year. Then she went through a seven-year period of what she calls a relative remission before falling ill again. She lives in Massachusetts and works from home as a writer and ME advocate, when she has energy.
Solomon represents most ME patients and advocates when she says that the amount of funding ME receives — even with new grants — is way too low.
Journalist Hillary Johnson compares ME to AIDS, for which funding increased drastically “once they realized it could be transmitted.” Many clinicians and researchers Johnson interviewed for “Osler’s Web” in the ’80s and ’90s believed ME had a contagious, infectious cause. In particular geographic locations around the world, doctors began seeing clusters of patients with crippling fatigue and neurological problems.
Now, HIV/AIDS receives about $3 billion in NIH funding each year for biomedical research on treatment, cure, prevention, and co-morbidities and co-infections. An estimated 1.1 million Americans have HIV. Adequate funding has led to HIV drug therapies that allow patients to lead semi-normal lives. ME is nowhere close to having a drug therapy, and its patients are crippled by bodies that cannot perform even minor tasks.
In 2018, still no cause — infectious or otherwise — has been found, even though thousands of papers have found biological abnormalities in ME patients.
Although new technologies and funding now exist, Solomon believes the real reason ME hasn’t been elucidated is that the federal government has failed to fund disease research in proportion to ME’s high burden of illness. This lack of funding hasn’t incentivized new researchers to study ME and has propagated the idea that ME is psychological, not physical, Solomon says. One highly visible study has helped promote the psychological theory of ME.
The controversial U.K. study, known as the PACE trial, was published in 2011, just seven years ago. The results of the $8 million experiments were similar to ME studies from the 1980s. PACE researchers asserted that ME patients had a false illness belief, making them reticent to exercise or lead a normal, healthy life, perpetuating feelings of illness. Patients could recover from this false belief, researchers said, through graded exercise therapy and cognitive behavioral therapy to help them realize they were not, in fact, ill at all.
An eight-week exercise program worsened Lizzie Mooney to the point that she was bedridden. And Amy Mooney cites another young patient whose goal for her exercise program was to overcome crippling stomach pain and stop using a wheelchair. The exercise made her sicker.
The PACE trial came under fire in 2015. David Tuller, a senior fellow in public health and journalism at the University of California, Berkeley’s School of Public Health, pointed out problems with the study that included author ties to disability insurance companies, a baseline scoring system that rated patients as simultaneously sick enough for the study yet healthy enough to be recovered, and a newsletter of patient testimonials released midway through the study that claimed benefits of the therapy.
“There could be 17 to 20 million of us or more around the world,” Solomon said, “and yet they still think we’re making this up.”
Millions needed

of Open Medicine Foundation, gives a
presentation. Her daughter fell ill in 2006
with sudden-onset ME. Tannenbaum has since
raised more than $13 million for research.
Advocates such as Linda Tannenbaum are concerned that some qualified ME researchers aren’t being funded by the NIH. In 2006, Tannenbaum’s daughter fell ill with sudden-onset ME. Tannenbaum, who lives in Agoura Hills, California, had worked in clinical lab science for over 23 years and had her own medical laboratory, but she’d never heard of ME. “We were told that she had something called chronic fatigue syndrome and there was nothing we could do for her other than pain management,” she said.
Tannenbaum set out to find a cure. By 2012, she had formed Open Medicine Foundation. She has since raised more than $13 million, much of it from the less-than-affluent patient community. An anonymous bitcoin philanthropist from the Pineapple Fund gave $5 million to OMF early in February.
“This disease is real, as emphasized by the caliber of researchers working together on this,” said Tannenbaum, who has helped to gather a global collaborative cohort of ME researchers.
OMF’s 15-member scientific advisory board includes three Nobel laureates and six National Academy of Science members. Hanson, from Cornell, is on the advisory board but her ME research is not funded by OMF.
Myalgic encephalomyelitis facts
| • Many ME patients report never recovering from a flu-like illness, a virus, a fever or some other infectious disease. • Patients must have symptoms for six months to be diagnosed with ME. • Up to three-quarters of patients spend a full year seeking a diagnosis; for 29 percent of patients, it takes more than five years. • ME affects both children and adults; 75 percent of adult patients are female. • While ME has been observed to persist following mononucleosis infection and has been referred to incorrectly as chronic mononucleosis, there is no evidence that ME is a form of mononucleosis. • Children experience some different ME symptoms from adults, with more frequent reporting of abdominal pain and rashes. • In one study, ME was the leading cause of prolonged sickness absence from school for children and staff in the U.K. |
• There still is not one diagnostic test specific to ME or one agreed-upon research case definition. • Two-day cardiopulmonary exercise tests, tilt table tests (where one lies on a table slowly tilted upward to measure how blood pressure and heart rate respond to gravity), and natural killer cell tests (which demonstrate reduced cytotoxicity in ME patients) have been used to indicate disease presence. • Cognitive dysfunction is well-documented as neurological impairment in ME patients. One study performed PET scans on ME patients and found cognitive impairment in ME patients correlated with brain areas such as the amygdala, thalamus and midbrain. • The majority of ME studies are done with a tiny cohort due to a lack of research funding. • The 2015 Institute of Medicine Report analyzed over 9,000 studies on ME and is a good source for a comprehensive ME literature review. |
Stanford University researchers, already funded by OMF for ME work, applied for but did not receive any of the new NIH grants. So the OMF leaders decided to fund another ME/CFS research center at Stanford University, supplying a grant starting at $1.2 million and continuing for as long as OMF can raise enough funds. More than 20 scientists will make up the OMF-funded center at Stanford, along with a growing working group of more than 30 researchers from top U.S. and international universities, who are not funded by OMF.
The Stanford ME center is led by ASBMB member Ronald W. Davis, director of OMF’s scientific advisory board and director of the Stanford Genome Technology Center. Davis’ son is severely ill with ME; he cannot leave his room, eat food or even speak. Davis has studied heavy metals and viruses in ME patients. He has coordinated a large -omics study on severely ill patients, a subgroup never studied before, analyzing genome sequences, proteins, metabolites, small RNA molecules and more. Severely ill patients are those who are homebound or bedbound, such as Davis’ son, who lacks the energy even to look at people. Davis hopes that his current and future research will help establish a large and open database where researchers can put new data to use in concert.
“People think they need to create their own big data and keep it to themselves, but this is expensive,” Davis said. “The rate-limiting step from publishing and getting ME research done is funding. I wish we had a lot more money to give everyone to make this much faster.”
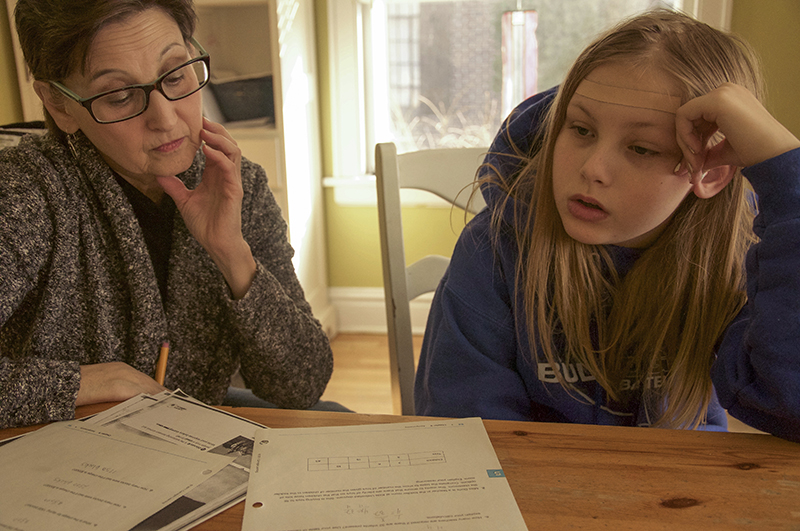
of her illness. She is pictured with her tutor, Judith Meyer.
The NIH was reluctant to fund his initial ME observational experiments, Davis said. But observation is needed before any hypotheses and future research directions can be established, he said, especially when so little observation has been done on ME. He hopes data he soon will publish will allow specialized researchers to study ME in their own fields, without the need to do costly and lengthy background research beforehand.
Jose Montoya, an ME physician and professor of medicine at Stanford, published a 2017 paper in the Proceedings of the National Academy of Sciences that analyzed an unusually high number of ME patients and controls as compared to typical ME studies: Serum from 192 patients and 392 healthy controls was analyzed for ytokine differences. Immune cells secrete cytokines, or cell-signaling molecules that play a role in inflammation. The signature flu-like symptoms and muscle pain led researchers to believe ME could be an inflammatory disorder.
Montoya and his team found that two cytokines were significantly different in ME patients and healthy controls. TGF-beta, found commonly in the monocytes and macrophages of the immune system as well as intestinal epithelial cells, is viewed as an anti-inflammatory cytokine. TGF-beta was higher in ME patients. Resistin, produced primarily by peripheral blood mononuclear cells, has been shown to increase transcription of pro-inflammatory genes and was lower in severe ME patients but higher in moderate ME patients. In total, Montoya’s study found 17 cytokines, 13 of which are pro-inflammatory, that had an upward linear trend when put into context of ME severity. In other words, these cytokines’ levels were higher in patients who had more severe symptoms. The study also cites resistin and another adipokine, leptin, as cytokines secreted by adipose tissue that could be important. Leptin has been found to correlate with fatigue severity, and levels are higher in females. Adipokines contribute to crosstalk between the central nervous system and adipose tissue and could contribute to neuroinflammation and cognitive dysfunction in ME patients. In mice, leptin has demonstrated a recruitment of neutrophils to the brain during sepsis, prompted by administration of lipopolysaccharide.
The new OMF-funded center at Stanford will have three main projects. One will explore the immunological basis of ME through analysis of T cells, the human immune cells that kill their infected own. ME could affect T-cell replication and behavior. This study also will investigate the way personal variations in human leukocyte antigen genes regulate immunity in ME patients. These genes code for the major histocompatibility complex, the cell-surface proteins that regulate our immune systems.
The second project will expand OMF’s current big-data genome study to patients of varying severities and their families, performing clinical and molecular tests that could provide insight into genetic factors and molecular biomarkers for ME. Right now, it has data from 20 ME patients. The third project will work toward a diagnostic that can distinguish ME blood samples from healthy ones using new technology developed at Stanford. The technology also will be used to test Food and Drug Administration–approved drugs considered for clinical trials on ME patients.

Don Mooney, share a laugh while studying a map on her bedroom wall.
“We need researchers to share their results openly and collaborate and look at ME/CFS through many body systems, genetics, infectious disease, immunology, metabolomics, microbiome and more,” Tannenbaum said. “The urgent need is not only research but awareness in the medical community and teaching new doctors in medical schools to be able to identify and acknowledge this.”
Far from treatment
Mary Dimmock, a 31-year veteran of the pharmaceutical industry, now retired, cites a significant roadblock to a treatment for ME: “Pharma has stayed away from this disease.”
During her time working for pharmaceutical companies, Dimmock did everything from drug metabolism studies to clinical data management to business process improvement initiatives. She saw the considerations that go into pharmaceutical companies’ research funding decisions. Before they even will think about investing in a particular drug or treatment, there must be potential patients for clinical trials, Dimmock says. To get a patient into a clinical trial, that patient must be diagnosed. But with ME, according to a 2015 Institute of Medicine Report, up to 91 percent of patients remain undiagnosed.
ME has numbers to support a huge market. “You’d think this would be a slam dunk for pharma,” Dimmock said. “But we don’t have agreement on a research definition, don’t have doctors treating patients and don’t have enough academic researchers.”
As someone who has seen what it takes to go from research to a marketable clinical treatment, Dimmock said she thinks the NIH has taken critical steps to attract more researchers and to promote collaboration. She also is encouraged by the work of the different centers, particularly Hanson’s focus on understanding the disease pathology after exercise studies.
Dimmock’s son has ME. She paid $65,000 out of pocket in the first year after his diagnosis. He eventually was able to use the two-day exercise study as a way to demonstrate disability.
But Dimmock, Solomon, Mooney and Johnson all worry that the NIH lacks any urgency, either in resolving the stigma of ME or in really ramping up funding. “Because they are taking one or two baby steps at a time, it will take more than a decade to get there,” Dimmock said.
Breen at NIH is aware that the agency’s decision-making process can take time and might seem a bit obscure. Every research application to the NIH must undergo a rigorous review by experts in the field, both by a scientific review group and by an institute’s advisory council or board. It typically takes about six months from the time an investigator submits an application, Breen said.
“The hard part for patients is that the timeline from research to a diagnostic test or therapeutic is never acceptable because there are people hurting now,” he said. “It looks very inefficient, but we have an open scope. We need to do more foundational studies for future diagnostics and therapeutics.”
Stanford’s Davis said understanding and urgency of funding for the disease are low because we just don’t see ME patients. They’re in their beds or at least at home. Trips to the hospital make them worse, so they don’t go. And although most patients aren’t dying from ME, they aren’t really living either.
“I understand the NIH’s predicament but I want them to take responsibility for this,” Davis said. “I know it’s hard. There are a lot of diseases out there and they’re probably all underfunded. But the NIH needs to serve the people of this country and that’s where the money is coming from, the people.”
Johnson is less forgiving. She remembers ME as a public health crisis. “In 10 years, a majority of people who came down with ME in the 1980s are likely to be dead. The shared memory of an epidemic beginning in the 1980s will be forgotten, and the government may never have to address its failures in the ’80s, ’90s and this century.”
Strides, albeit small, are being made by researchers, who now recognize the role of the microbiome, immune and nervous systems, and metabolism. The number of ME researchers is growing, even with limited funding.
With at least 17 million to 20 million estimated patients around the globe, a researcher entering the field now could “make their mark with minimal effort,” Solomon said. Dimmock would agree. “While I appreciate the risk from a pharmaceutical perspective, the time is ripe for academics to get interested in ME,” she said. “It is a fascinating biological mystery.”
“Here is your chance,” Davis tells his students at Stanford.
February marked year three of Lizzie’s illness. She hopes ME’s mysteries are unraveled soon, so she can trade her Chicago Bears pajamas for jeans and sneakers, leave her bedroom, and go back to school.
Advocating for their lives

to leave their beds and join the action. This photo was taken in Birmingham, England.
While researchers funded by the federal National Institutes of Health and the private Open Medicine Foundation embark on studies paid for by new grants, patients and advocates continue the push to make myalgic encephalomyelitis more visible.
They spent months organizing dozens of rallies around the world in 2016 and 2017, hoping to raise awareness about ME. Amy Mooney wielded a megaphone in downtown Chicago as part of that #MillionsMissing campaign, which laid out a pair of shoes for each ME sufferer too sick to attend in person. The ground was a sea of shoes no longer worn by their homebound owners. Another rally is being organized for this May.
The 2017 documentary “ Unrest” chronicles the life of Jennifer Brea, an ME patient who is also the film’s producer. It has won or been nominated for more than a dozen awards and recently aired on PBS. Rivka Solomon organized a screening of “Unrest” in November that attracted an audience of 363 — about 100 of whom were Boston healthcare professionals — and was the largest community screening of the film to date. This event earned a statement of support for ME patients from the entire Massachusetts congressional delegation.
“In just the past half-year the film, “Unrest,” is shifting the landscape for us,” Solomon said. “But before that, I would say not much changed for us for 30 years.” She would know; she has been sick for 28.
Solomon also found a champion in Sen. Ed Markey, a Massachusetts Democrat, who held a congressional briefing about ME on Capitol Hill in May 2017.
In Illinois, Amy Mooney worked to pass a proclamation in the state’s House of Representatives, affirming the state’s commitment to improving quality of care for ME patients. The House encouraged the media to cover the disease and Illinois universities to study ME, recommending that the NIH proportionately fund research and that the Centers for Disease Control and Prevention disseminate proper information. Mooney also hosted a screening of “Unrest” in the Chicago suburb where she lives.
“They’re not promising money or anything at this point,” Mooney said, “but we want universities to say, ‘Oh, this is real,’ and it to be something they respond to and investigate.” Mooney used to be able to work, but now her full-time job is advocating on behalf of her 12-year-old.
Journalist Hillary Johnson continues to report on her website.
“By and large, each time I do something for ME advocacy, I pay a price,” Solomon said. “I often end up much sicker than before, and I never know for how long I’ll be in the relapse. It’s pretty scary that advocating for your own life can cause such a detrimental setback in your health. I call this our fundamental conundrum.”
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

Unraveling oncogenesis: What makes cancer tick?
Learn about the ASBMB 2025 symposium on oncogenic hubs: chromatin regulatory and transcriptional complexes in cancer.

Exploring lipid metabolism: A journey through time and innovation
Recent lipid metabolism research has unveiled critical insights into lipid–protein interactions, offering potential therapeutic targets for metabolic and neurodegenerative diseases. Check out the latest in lipid science at the ASBMB annual meeting.

Melissa Moore to speak at ASBMB 2025
Richard Silverman and Melissa Moore are the featured speakers at the ASBMB annual meeting to be held April 12-15 in Chicago.
A new kind of stem cell is revolutionizing regenerative medicine
Induced pluripotent stem cells are paving the way for personalized treatments to diabetes, vision loss and more. However, scientists still face hurdles such as strict regulations, scalability, cell longevity and immune rejection.

Engineering the future with synthetic biology
Learn about the ASBMB 2025 symposium on synthetic biology, featuring applications to better human and environmental health.

Scientists find bacterial ‘Achilles’ heel’ to combat antibiotic resistance
Alejandro Vila, an ASBMB Breakthroughs speaker, discussed his work on metallo-β-lactamase enzymes and their dependence on zinc.

