Counting carbs
Which is better for you: a sugary cereal or a baked potato? According to the glycemic index, the cereal would win because it scores lower.
Since its inception in 1981, the glycemic index — a measure of the changes in blood-glucose levels in response to the consumption of a food containing carbohydrates — has been a source of contention.
Experts tend to fall into one of two camps. One camp believes that a low-glycemic-index diet helps weight loss and keeps chronic illnesses, such as cardiovascular disease, Type 2 diabetes and age-related macular degeneration, at bay. This camp has been pushing for labeling foods with their GI values. The index has been used as the basis of several commercial diets, including the Nutrisystem diet, which has been endorsed by celebrities such as Marie Osmond and Dan Marino.
The other camp counters that glycemic index doesn’t clearly delineate between healthful and unhealthful foods: Because some junk foods show up on the lower end of the GI scale, which is thought to be better, the critics argue, the glycemic index confuses consumers. They also contend that the evidence for the health benefits of the glycemic index just isn’t consistent. Joanne Slavin at the University of Minnesota was part of the 2010 committee that did the most recent analysis of the U.S. dietary guidelines. “We did the review on GI,” she says. “There was strong evidence that the GI isn’t linked to health outcomes in healthy people.” (See the excerpt from the 2010 U.S. dietary guidelines below.)
This summer, the regulatory authority Health Canada issued a white paper to say that it has decided the index is not going to be put on food labels in Canada. “GI is confusing,” says Alfred Aziz of Health Canada, the first author on the paper. “We don’t feel it’s a good labeling measure.” Health advocacy organizations in the U.S., such the American Heart Association and the American Diabetes Association, haven’t yet adopted the glycemic index. The Canadian Diabetes Association has advocated that Type 1 and 2 diabetics use the measure in its 2013 Clinical Practice Guidelines.
Supporters of the index decry Health Canada’s decision as well as the judgments of the glycemic index detractors. “The criticisms are uninformed,” says Jennie Brand-Miller, director of the University of Sydney’s GI testing service, SUGiRS. She and others believe that unfortunate circumstances have the plagued glycemic index. “Some of it is the politics of food, and some of it is the politics of science,” says Brand-Miller. “Some of the controversy is because GI didn’t come out of America. It was from Canada and Australia, and that set up these opposing forces.” (See box for all sources’ conflicts of interest.)
What is the glycemic index?
The GI is a measure that ranks foods containing carbohydrates according to their potential to raise blood-glucose levels after being consumed. To get a measure of a food’s GI, participants in a study are given the test food to eat. The test food contains a known amount of carbohydrate, usually 50 or 100 grams. The participants’ blood-glucose levels are measured by finger-prick tests over the course of two hours after they’ve consumed the food. Then, on three different days, the participants are given the equivalent amount of glucose powder dissolved in water, which acts as a reference. (Sometimes, researchers use white bread).
 The changes in blood-glucose level after eating the test food are plotted as a function of time, and the area under the curve is calculated. The same is done for glucose. The value of the area under the curve for the test food is divided by the average value of the areas under the curve for the reference and then multiplied by 100. The resulting number is a unitless measure, a ratio of the blood-glucose response between the test and reference sample.
The changes in blood-glucose level after eating the test food are plotted as a function of time, and the area under the curve is calculated. The same is done for glucose. The value of the area under the curve for the test food is divided by the average value of the areas under the curve for the reference and then multiplied by 100. The resulting number is a unitless measure, a ratio of the blood-glucose response between the test and reference sample.
Foods that score 70 and above are classified as high on the glycemic index. Foods that score 55 or less are classified as low, and those in the middle are classified as medium.
A personal response?
Because the measurement is done in people, critics argue that this makes the glycemic index susceptible to variation.
People who want to push the glycemic index make claims on the assumption it’s an absolute quantity, which is dependent entirely on the food that you’re eating and does not reflect in any way a person’s metabolism,” says William Whelan at the University of Miami. “They are assuming that it doesn’t matter who you are — if you eat this particular food, you’re going to get this particular glycemic response. That’s nonsense.
Whelan’s view is that glycemic response is highly specific to how an individual processes carbohydrates. The rise in blood glucose “causes a release of insulin. Insulin then works to drive the glucose in the direction of fat synthesis,” says Whelan. “The extent to which that affects any individual depends on his or her own individual glycemic response.
Whelan’s research has shown that a person has a set baseline in his or her response to carbohydrates. Two people can eat the same quantity of the same food, but one person can have a higher spike in blood-glucose level than the other person. This observation, which he made in healthy undergraduate students recruited from the University of Miami, cuts across all kinds of carbohydrate-containing foods.
Whelan asserts that proponents of low-GI diets don’t acknowledge this biological fact. “Their message is valid only for that section of the population that naturally, from their own metabolism, for whatever reason, has a low glycemic response to whatever they eat.
But Brand-Miller counters that the GI holds steady across different population subsets. “We’ve been able to show that if a food is low GI in a normal, healthy young individual it’s also low GI in elderly people, children, people with impaired glucose tolerance or people who are overweight.
Thomas Wolever at the University of Toronto says that critics confuse the glycemic index with the glycemic response. “Often times, when people criticize GI, they are not actually talking about GI. They are talking about a glucose response.
Excerpt from the 2010
U.S. Dietary Guidelines
Strong and consistent evidence shows that glycemic index and/or glycemic load are not associated with body weight and do not lead to greater weight loss or better weight maintenance. Abundant, strong epidemiological evidence demonstrates that there is no association between glycemic index or load and cancer. A moderate body of inconsistent evidence supports a relationship between high glycemic index and Type 2 diabetes. Strong, convincing evidence shows little association between glycemic load and Type 2 diabetes. Due to limited evidence, no conclusion can be drawn to assess the relationship between either glycemic index or load and cardiovascular disease.
Source: http://1.usa.gov/1gnFLVa
Variation is a sticking point
Health Canada pointed to variation when it decided against printing GI values on food labels. “Compared to other measures of food, for example lipids or proteins, where you actually measure them in instruments, the instrument for the glycemic index is the individual,” says Aziz. “You can appreciate how you can have such a large variation when you use a person as an instrument to measure a property of the food.
David Jenkins at the University of Toronto and other proponents of GI say the variation issue is overblown. “There are individual differences, but they are not big,” states Jenkins, who, along with Wolever, first published the concept of GI. “The big difference is basically a difference between my glucose tolerance and yours when it’s not indexed” to glucose. What matters, says Jenkins, is the collective response of a group of people to a particular food in comparison with their response to a reference food.
Proponents of the glycemic index are very much aware that people differ, even day to day. “The human instrument is very imprecise,” says Wolever. “But we’ve developed the method to take that into consideration.
Wolever says his group measures the reference food more than once, because its value is the denominator in the calculation. “We have to measure it several times to try to get a better representation of that subject’s true response, because it varies tremendously from day to day,” he says. “The GI value you get depends more on the denominator than the numerator. That’s why the denominator is important. That is lost on people.
But Aziz counters that the multiple measurements of the reference food don’t cut it. Despite the multiple measurements and averaging, he says, “it’s still a highly variable measure.
Meaningful measurement
Making a reliable measurement can be problematic. Slavin uses carrots as the example. “For me to deliver 100 grams of carbohydrate in the form of carrots in a feeding study, that’s like 15 servings,” she says. “It’s a huge pile of carrots, because you’ve got to come up with 100 grams! Carrots are mostly water, a little bit of fiber and a little bit of starch. The GI is very nonrepresentative of what people actually eat.
Also, values reported for a given food can be all over the map. Slavin goes back to her carrots example. GI values reported for carrots in the literature “can go anywhere from 50 up to 120. It’s all over the place,” says Slavin. “There is no government standard of the use — to say ‘This is the value for carrots’ — because there isn’t a value. It’s a moving target.
GI supporters agree there is a problem with consistency: The literature is littered with different values for the same foods, because the studies didn’t follow the same methodology. Part of the problem with the GI literature is that “the amounts of carbohydrate in the studies vary,” says Wolever. “When you look at nutrition studies, they are not all the same. It’s not like a drug study.
The other problem is the food itself, says Jenkins. Processed foods are being reformulated continuously. This means measurements made with previous iterations of a product become useless. “We’ve got a real problem with changing food supplies,” says Jenkins. “Imagine if you’re responsible for trying to keep a database of foods that have all been tested for groups of healthy individuals. How can you keep that database up to date and relevant?
Another problem “stems from the fact that we’re often looking at small differences in GI. You need very large numbers of people to show differences in outcome,” says Jenkins. Aziz adds that many studies also don’t pay attention to the race and ethnicity of the participants. People of different racial and ethnic backgrounds are known to have different metabolic patterns. “Ideally, you need to have equal representation of different ethnic groups in your sample size to be able to have a more meaningful and accurate GI value,” says Aziz. With researchers using a few individuals in their studies and old GI measurements, Jenkins says, it’s not surprising that the data are riddled with problems.
Jenkins argues that GI becomes most important in people who suffer a metabolic disorder. He says that much of the controversy surrounding GI is rooted in the fact that many of the studies were done in healthy individuals who probably can weather the ups and downs of diet better than people with some sort of disorder. For better assessments of the impact of GI, “don’t try looking at healthy people. You’ll find it very difficult, because nothing makes much of a difference. They’ve already got very good insulin and glucose tolerance. There’s not much room to change,” says Jenkins. “The worse shape you’re in, the more you’re going to magnify the effects” of changing your diet.
Perhaps that is why the Canadian Diabetes Association concluded in its 2013 Clinical Practice Guidelines, “Meta-analyses of controlled feeding trials of interventions replacing high-GI (carbohydrates) with low-GI (carbohydrates) in mixed meals have shown clinically significant improvements in glycemic control over 2 weeks to 6 months in people with Type 1 or Type 2 diabetes … This dietary strategy also leads to improvements in cardiovascular risk factors” (2).
Other issues
GI doesn’t capture the interactions of other foods, the critics object. “You never consume foods by themselves,” Slavin notes. “If you eat a piece of bread, you probably have butter or peanut butter on it. The GI is much lower because you’ve put fat on it.” Fat is thought to slow down the breakdown of foods and the release of glucose.
The glycemic index’s supporters counter this notion. “They will say when you add butter to bread, you change its glycemic index. You don’t,” counters Wolever. “Bread is bread! Its GI hasn’t been changed. The glycemic impact of the meal has been changed.
Because the index is simply a measure of blood-glucose levels in response to a known amount of carbohydrate, everything else, such as protein and fat, is not considered. For this reason, critics say a pizza can have a low-GI crust but then have salty and fatty ingredients, such as pepperoni and cheese, as toppings, which won’t count toward the index.
The fact that unhealthy foods can appear with low GI values is a big concern, say the critics. The example repeatedly brought up is fructose, found in many processed foods. Upon ingestion, fructose goes to the liver and enters the glycolytic pathway. “It elicits a low glycemic response, and hence it has a low GI value,” says Aziz. Because of that, a can of soda, which contains fructose and glucose, can have a lower GI value than a baked potato, which is mostly starch that gets broken into glucose.
The subject of junk food exasperates Wolever. “We’re not talking about chocolates! That’s not the point,” he says. “Let’s look at our staple carbohydrates, the things we’re supposed to be getting 45 (percent) to 60 percent of our energy from, and which one of those are the ones with a low GI. Those are ones that we should be focusing on.
But the detractors counter that that doesn’t help the public seeking a label to help them decide what to eat. Slavin says the glycemic index makes it hard to send a one-size-fits-all message. Its message is more nuanced — that certain carbohydrates with particular glycemic index values should be chosen over others.
Brand-Miller disagrees that the message is complicated. “My message is simpler than you think. People don’t have to remember a whole lot of numbers. There’s a need for food labeling,” she says. “Just exchange a high-glycemic-index bread for a low-glycemic-index bread, and the same thing for breakfast cereal and rice. Try to have more of the lowest-glycemic-index foods, like legumes, pasta and dairy.
Health benefits?
Despite doubts about the usefulness of the GI on food labels, experts say the index is useful to explore how diet affects health outcomes in a research setting. For example, Allen Taylor at Tufts University is interested in the link between a high-glycemic-index diet and glycation of proteins. Sugars can react with proteins through the Maillard reaction to produce advanced glycation end products, which “accumulate with accelerating rates with age,” explains Taylor. The implication is that these accumulated glycated end products jam up the proteolytic machinery.
If you feed animals high-glycemic-index diets, sure enough, they accumulate these glycation products throughout their whole bodies, even though they are not diabetic,” says Taylor. These glycated products are thought to be cytotoxic, and because they are produced indiscriminately throughout the body, they have effects away from the central metabolic pathways in the gut and liver. Taylor says his group has collected similar data from human studies: People who consume high-glycemic diets develop cataracts, age-related macular degeneration, diabetes and cardiovascular disease at higher rates than normal. “There are seemingly systemic effects of the stress that’s caused by diets that deliver sugar rapidly,” Taylor says.
Brand-Miller explains the mechanism for Type 2 diabetes. “Beta cells are the most sensitive cells in the body from the point of view of detecting glucose.” She adds that the mitochondria “are producing lots of NADH and free radicals when the glucose load is very high. It overwhelms the capacity of the beta cells to quench the oxidative stress.
But more studies, on larger scales, have to be done. According to the 2010 U.S. dietary guidelines, “A moderate body of inconsistent evidence supports a relationship between high glycemic index and Type 2 diabetes … Due to limited evidence, no conclusion can be drawn to assess the relationship between either glycemic index or load and cardiovascular disease.

Declared conflicts of interest and financial gains
- Jennie Brand-Miller is president of a nonprofit glycemic-index-based food-endorsement program called the Glycemic Index Foundation and the director of the University of Sydney’s GI testing service, SUGiRS. She is a co-author of “The Glucose Revolution” and “The New Glucose Revolution” book series (Marlowe and Co., New York) and “The Low GI Diet” book series (Hachette Australia).
- Thomas Wolever is the president, the medical director and a scientist at Glycemic Index Laboratories Inc., a contract research organization. He is also president and an owner of Glycaemic Index Testing Inc., which provides services to GI Labs. He receives royalties as co-author of a number of books on GI under the general title of “The Glucose Revolution” and consulting fees from Tamasek Polytechnic for advice related to GI research. In the past three years, he has consulted for McCain Foods Inc. and Bunge.
- David Jenkins consults with and has accepted funding from numerous food companies and organizations, such as Barilla, Kellogg’s, Quaker Oats, Coca-Cola, The California Strawberry Commission and Agrifoods and Agriculture, Canada. His wife, Alexandra Jenkins, is director and partner with Wolever at the Glycemic Index Laboratories, which tests foods that Jenkins uses in his studies.
- William Whelan has accepted funding for his GI research from the Agatson Foundation, established by Arthur Agatson, who developed the low-carbohydrate South Beach Diet. He also has co-authored a paper on GI with Agatson (IUBMB Life. 62, 637 – 641 (2010)).
- Alfred Aziz, Joanne Slavin and Allen Taylor declared no conflicts of interest.
Improving the index
Wolever, Brand-Miller and Jenkins say that the arguments that have dogged GI for the past 30 years need to be laid to rest so that the field can move forward. In their view, the criticisms are old and have been refuted by their research. The most important thing now, Wolever says, is making the measurement and application of GI consistent to avoid further obfuscation.
Experts agree that any measure that helps people make better dietary choices is a good one to have. “We acknowledge that carbohydrate-rich foods that result in a lower blood-glucose response or can mitigate the glycemic response after a meal would be beneficial in general,” Aziz says. For this reason, he says, Health Canada is developing a guidance document that sets out the criteria for establishing a health claim that the consumption of a food leads to a reduced glycemic response.
The critics agree with Health Canada’s assessment. “Everybody wants a measure of carbohydrate quality. I get that,” says Slavin. “The glycemic index appears like a good measure.” But the problem is that GI doesn’t distinguish between healthful and junk foods. As Slavin sums it up, “The glycemic index doesn’t really drive the foods we want people to consume more.

Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles
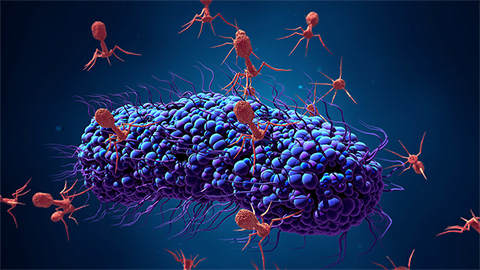
Bacteriophage protein could make queso fresco safer
Researchers characterized the structure and function of PlyP100, a bacteriophage protein that shows promise as a food-safe antimicrobial for preventing Listeria monocytogenes growth in fresh cheeses.

Building the blueprint to block HIV
Wesley Sundquist will present his work on the HIV capsid and revolutionary drug, Lenacapavir, at the ASBMB Annual Meeting, March 7–10, in Maryland.
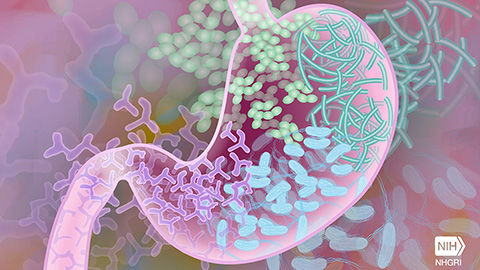
Gut microbes hijack cancer pathway in high-fat diets
Researchers at the Feinstein Institutes for Medical Research found that a high-fat diet increases ammonia-producing bacteria in the gut microbiome of mice, which in turn disrupts TGF-β signaling and promotes colorectal cancer.

Mapping fentanyl’s cellular footprint
Using a new imaging method, researchers at State University of New York at Buffalo traced fentanyl’s effects inside brain immune cells, revealing how the drug alters lipid droplets, pointing to new paths for addiction diagnostics.

Designing life’s building blocks with AI
Tanja Kortemme, a professor at the University of California, San Francisco, will discuss her research using computational biology to engineer proteins at the 2026 ASBMB Annual Meeting.
Cholesterol as a novel biomarker for Fragile X syndrome
Researchers in Quebec identified lower levels of a brain cholesterol metabolite, 24-hydroxycholesterol, in patients with fragile X syndrome, a finding that could provide a simple blood-based biomarker for understanding and managing the condition.

