From the journals: JLR
Muscle lipids and metabolic syndrome. A new method for detecting peroxisomal disorders. Testing oligonucleotide therapy in NASH. Read about papers on these topics recently published in the Journal of Lipid Research.
Muscle lipids and metabolic syndrome
Metabolic syndrome represents a combination of conditions that co-occur, heightening the likelihood of heart disease, stroke and Type 2 diabetes. It's also known as syndrome X or insulin resistance, embodying a pathological condition characterized by elevated blood pressure, heightened blood sugar levels, surplus abdominal fat and abnormal cholesterol or triglyceride levels. Skeletal muscle insulin resistance refers to insulin's inability to adequately stimulate glucose uptake into skeletal muscle. Skeletal muscles play a vital role in regulating glucose levels by responding vigorously to insulin and storing most cleared glucose as glycogen. Thus, muscle insulin resistance is a critical factor that impacts overall insulin resistance and blood glucose levels.
In a recent article published in the Journal of Lipid Research, Samantha Adamson and her team at Washington University in St. Louis, examined the roles of phosphatidylcholine, or PC, phosphatidylethanolamine, or PE, and PC to PE ratios in skeletal muscle sarcoplasmic reticulum in metabolic syndrome. The sarcoplasmic reticulum, or SR, is a storage unit within muscle cells that holds and releases calcium ions, which are crucial for muscle contraction.
Previous studies in humans have examined phospholipids in whole-muscle lysate rather than specific subcellular compartments. In this study, the authors correlated PC and PE composition in vastus lateralis muscle SR fractions between sedentary individuals with metabolic syndrome and sedentary lean controls. They report that compared to sedentary lean controls, total PC and PE levels were notably reduced in muscle SR in individuals with metabolic syndrome. However, they discerned no distinction in the PC to PE ratio between the two groups. Reduced SR PC, but not PE levels correlated with increased body mass index, waist circumference, total fat and insulin resistance.
This study sets the stage for understanding the precise role of SR phospholipids in the regulation of insulin-mediated glucose disposal in the skeletal muscle.
New method for detecting peroxisomal disorders
Peroxisomal disorders, or PDs, such as X-linked adrenoleukodystrophy, or ALD, and Zellweger syndrome, or ZS, encompass a spectrum of genetically diverse metabolic conditions characterized by malfunctioning peroxisomes. Peroxisomes are instrumental organelles that aid in the β-oxidation of very long-chain fatty acids, or VLCFAs which contain more than 22 carbons, and hydrogen peroxide detoxification. Various PDs require distinct treatments, so accurate diagnosis is critical.
Genetic defects in peroxisomal β-oxidation lead to VLCFA accumulation, triggering health problems, including nervous tissue demyelination. To diagnose peroxisomal disorders, physicians often measure plasma levels of VLCFAs. Quantifying VLCFAs through direct transesterification followed by gas chromatography analysis has performed exceptionally for decades, establishing it as the gold standard for diagnosing PDs; however, it is a time-consuming and labor-intensive procedure. In a recent study published in the Journal of Lipid Research, Blai Morales–Romero and his team at the Center for Biomedical Research Network on Rare Diseases in Spain, report that very long-chain lysophosphatidylcholine, or LPC, levels, measured by liquid chromatography with tandem mass spectrometry, may be an alternative, faster approach to diagnose PDs.
The team’s results showed they could detect LPCs with greater accuracy than traditional plasma VLCFAs, especially in ALD females. The authors suggest using the analysis of VLCFA to LPC ratios as potential tools for differentiating ALD from ZS. The authors call for more extensive studies involving diverse patient groups to validate and broaden these findings and improve PD diagnosis.
Testing oligonucleotide therapy in NASH
Nonalcoholic steatohepatitis, or NASH, is a fatty liver disease characterized by liver inflammation that may progress to severe conditions such as fibrosis, cirrhosis and even liver cancer over time. The 17-beta hydroxysteroid dehydrogenase 13, also called HSD17B13, is a liver-enriched protein associated with lipid droplets. HSD17B13 has been strongly linked to the progression and development of NASH in humans and mice. While the exact role of HSD17B13 in NASH is unclear, antisense oligonucleotides, or ASOs, and small interfering RNA Hsd17b13 inhibitors are already in clinical trials for treating this disease.
In a recent study published in the Journal of Lipid Research, Yanling Ma and a team at Bristol Myers Squibb provide insights into the benefits and limitations of targeting Hsd17b13 in treating NASH. To mimic the fibrosis aspect of human NASH, a disease hallmark, the team used mice fed a choline-deficient, L-amino acid–defined high-fat diet, or CDAHFD. The team's experimental approach involved targeting Hsd17b13 using ASOs in CDAHFD mice. However, despite significantly reducing the levels of Hsd17b13 messenger RNA, the approach failed to reduce hepatic fibrosis in the CDAHFD-fed mice at any administered dose.
Ma and colleagues concluded that further research is needed to evaluate the role of HSD17B13 in NASH. They suggested that future studies should explore therapies that reduce NASH fibrosis in humanized animal models, such as alternative ASOs for Hsd17b13. The study underscores the need for preclinical studies validating the use of Hsd17b13 ASOs in NASH progression before clinical trials.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles
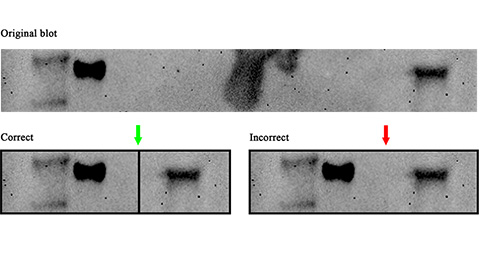
Avoiding common figure errors in manuscript submissions
The three figure issues most often flagged during JBC’s data integrity review are background signal errors, image reuse and undeclared splicing errors. Learn how to avoid these and prevent mistakes that could impede publication.
Ragweed compound thwarts aggressive bladder and breast cancers
Scientists from the University of Michigan reveal the mechanism of action of ambrosin, a compound from ragweed, selectively attacks advanced bladder and breast cancer cells in cell-based models, highlighting its potential to treat advanced tumors.
Lipid-lowering therapies could help treat IBD
Genetic evidence shows that drugs that reduce cholesterol or triglyceride levels can either raise or lower inflammatory bowel disease risk by altering gut microbes and immune signaling.
Key regulator of cholesterol protects against Alzheimer’s disease
A new study identifies oxysterol-binding protein-related protein 6 as a central controller of brain cholesterol balance, with protective effects against Alzheimer’s-related neurodegeneration.

From humble beginnings to unlocking lysosomal secrets
Monther Abu–Remaileh will receive the ASBMB’s 2026 Walter A. Shaw Young Investigator Award in Lipid Research at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

Chemistry meets biology to thwart parasites
Margaret Phillips will receive the Alice and C. C. Wang Award in Molecular Parasitology at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

