St. Jude and maximizing the value of blood
About 6.8 million people donate blood in the U.S. every year. How we envision our blood being used is predominantly shaped by movies or television shows, depicting frantic emergency rooms and injuries requiring immediate blood transfusion. As testament to this, nothing drives us to donate blood more than a disaster. This is only natural — at our core we are a hugely empathetic species. But this generosity can often be misguided.
More than 200,000 units of whole blood had to be thrown out after the Sept. 11, 2001, terrorist attacks drove an unprecedented number of Americans to their local blood donation centers. But what about when there is no pertinent drive to get us to give up our blood? What about those individuals whose daily need for blood donations often gets forgotten?
At St. Jude Children’s Research Hospital in Memphis, some 7,500 patients are treated for childhood cancers and other catastrophic diseases based on the wish of its founder, Danny Thomas, that “no child should die in the dawn of life.” While the hospital’s achievements in the goal of improving childhood cancer survival rates are countless, perhaps what St. Jude is most renowned for is that none of the costs of treatment get passed on to the families. To facilitate this, the in-house capabilities of St. Jude are second to none. This includes the on-site blood donation facilities.

‘Very low wastage’
The roles of the St. Jude Therapeutic Apheresis and Blood Donor Center are directly linked to needs of the patients of the hospital. Along with blood donations, the center facilitates therapeutic plasma exchange, photopheresis (isolation of white blood cells), red cell exchanges, stem cell transplants and granulocyte exchanges.
At the core of these processes is apheresis. Apheresis is the practice of separating blood drawn from a donor into its individual components — plasma, red and white blood cells, and platelets — taking what is needed and returning the rest to the donor.
Since St. Jude is a specialized hospital, emergency blood transfusions are not the primary destination for donated blood; in fact, St. Jude does not even have need of a dedicated ER.
The blood product most in demand at St. Jude are the precious platelets. Patients receiving chemotherapy very often see their platelet-producing bone marrow cells damaged by the process. It is therefore imperative to have a constant supply of platelets since they act as the body’s clotting factor.
The kicker? Platelets don’t do very well in the cold, unlike their red blood cell counterparts. A donation of platelets is only good for five days before it expires. This means the donation center must meet constantly updating goals so as to keep up with the demand of the hospital. And they have this process down to a fine art.
“All blood products drawn at St. Jude are for St. Jude patients. We don’t even have a license to ship. This is the way St. Jude operates,” Deirdre Cullen, manager at the blood donation center explained. “There’s very low wastage — we take what is needed from the blood, and the doctors and nurses schedule so they can get what they need, when they need it. It’s kind of like a boutique: Whatever the doctors and nurses might need, we get it for them. Less than 1% wasted a month.”
Sickle cell clinical trial
The center also supplies samples for the wide range of biomedical research done at St. Jude.
Among other blood disorders, sickle cell disease was immediately identified as an acutely important research target for the hospital. The genetic disease, which affects hemoglobin, is named for the distinct sickle shape that red blood cells subsequently adopt. This misshapen cell slows movement of blood through blood vessels, slowing the movement of oxygen around the body.
About 1 million to 3 million Americans are affected, with significant demographic disproportion (roughly 8% to 10% of African-Americans are carriers of the sickle cell trait). While treatment is available, more viable therapies to cure the disease are now being investigated.
Recently, researchers took advantage of an observation made back in 1948: fetal hemoglobin does not bring about sickle shape cells. This led to the development of a genetic therapy to restore production of fetal hemoglobin. St. Jude is one of several hospitals where patients have participated in this trial.
Treatment involves separation of a patient’s blood stem cells from the rest of the blood (via apheresis). The CRISPR–Cas9 gene-editing system is then used to edit a noncoding region in the BCL11A gene, which naturally functions as a silencer for fetal hemoglobin, restoring the cell’s ability to produce it again.
The cells are then given back to the patient in a process called a hematopoietic stem-cell transplant after the patient is conditioned through a round of chemotherapy.
This study is estimated to be completed in May 2022, but patients at St. Jude are already seeing the benefits of such next-generation therapies.

Well-oiled machine
To ensure the supply of blood products never runs out, St. Jude donors are handled a bit differently than those who donate via other organizations, such as the Red Cross.
It is important for the hospital to space out the donations and time them correctly to ensure a year-round supply of all blood products, with a loyal register of donors in case a particular blood type or HLA-matched platelets is needed at short notice.
The conductors of this process are Kimberly Spencer Foster and Karen Wimpee.
“We get a spreadsheet for the month outlining what we need to reach as a goal. Then we look at what we have, see what expires today, tomorrow, the next day, etc. It is a continuous system,” explained Foster. “We want you when your product can be put to its best use.”
Currently, the center aims to draw 11 units of platelets a day, with each unit ranging in value from $400 to $600.
And as Wimpee emphasized, “bringing the donors in to St. Jude to give blood allows the hospital to cut down on the cost associated with purchasing blood from outside.”
A community united
COVID-19 has created some expected hurdles, including vaccine hesitancy, room occupancy limits and other safety measures.
When the pandemic first hit, St. Jude took donations only from the hospital staff, who receive weekly COVID tests on site. But donations have now opened back up to the public.
Thankfully, platelet donations have dropped only modestly — from 2,480 in 2019 to 2,430 in 2020. Cullen credits community support for helping to maintain the hospital’s blood supply. “People had more time; everyone was at home! And the community just wanted to help out however they could,” she said.
This was not necessarily the case nationally however, as recent Red Cross reports suggest donor numbers have dropped while the demand for blood products has increased.
Dedicated donors
The business-as-usual response to the pandemic is testament to the dedication of the staff, as well as the loyal donor base.
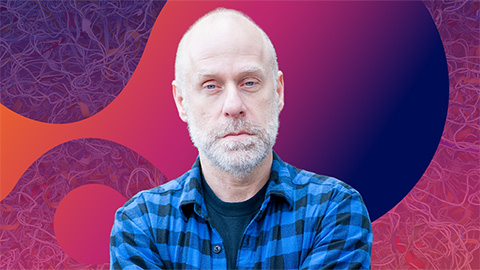
This loyalty is epitomized by Chris Clark, who is approaching his 500th donation since 1996, which equates to about 20 donations a year for 25 years (platelets can be donated up to 24 times a year).
The longest active donor at St. Jude has been donating since 1976.
The hospital also recently celebrated the life of its oldest donor, who donated every two weeks until he was 87.
While all blood donations are gifts, those who stop by the hospital to donate have the added assurance of knowing their donations never leave the campus and will go directly to helping the children there.
Learn how to become a donor for St. Jude.
If you are not in the Memphis area to donate, please consider seeing your local options for donation here or here.

Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreFeatured jobs
from the ASBMB career center
Get the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

Life in four dimensions: When biology outpaces the brain
Nobel laureate Eric Betzig will discuss his research on information transfer in biology from proteins to organisms at the 2026 ASBMB Annual Meeting.

Fasting, fat and the molecular switches that keep us alive
Nutritional biochemist and JLR AE Sander Kersten has spent decades uncovering how the body adapts to fasting. His discoveries on lipid metabolism and gene regulation reveal how our ancient survival mechanisms may hold keys to modern metabolic health.

Redefining excellence to drive equity and innovation
Donita Brady will receive the ASBMB Ruth Kirschstein Award for Maximizing Access in Science at the ASBMB Annual Meeting, March 7–10, just outside of Washington, D.C.

Mining microbes for rare earth solutions
Joseph Cotruvo, Jr., will receive the ASBMB Mildred Cohn Young Investigator Award at the ASBMB Annual Meeting, March 7–10, just outside of Washington, D.C.

Fueling healthier aging, connecting metabolism stress and time
Biochemist Melanie McReynolds investigates how metabolism and stress shape the aging process. Her research on NAD+, a molecule central to cellular energy, reveals how maintaining its balance could promote healthier, longer lives.
Mapping proteins, one side chain at a time
Roland Dunbrack Jr. will receive the ASBMB DeLano Award for Computational Biosciences at the ASBMB Annual Meeting, March 7–10, just outside of Washington, D.C.

