How chronic pain shows up in urine
Chronic pain diseases are underresearched — particularly for women, particularly with pelvic pain. Almost certainly, someone you know suffers from this. For people with urinary chronic pelvic pain syndrome, or UCPPS, the need to urinate is particularly frequent or urgent, or pelvic pain is prominent, or both. It’s often simply a diagnosis of exclusion, and there is a lack of effective treatments.

Using protein signatures in urine, researchers have been able to distinguish UCPPS from other chronic pain diseases, including myalgic encephalomyelitis/chronic fatigue syndrome, or ME/CFS, as well as fibromyalgia and irritable bowel syndrome.
According to a recent article in the journal Molecular & Cellular Proteomics, lurking in urine all along were pronounced differences in the proteins related to chronic pain for different sexes — and leads for diagnosis and treatment.
We often think of pain in terms of blunt force, but the workings of chronic pain are more like pulling thousands of tiny strings in the theater of a cell. To develop new treatments and diagnostics, we need to know which proteins are pulling strings or playing other parts.
Finding those proteins is the most powerful aspect of this study, according to first author John Froehlich, professor of surgery at Harvard Medical School. He said his team is “measuring the real things that carry out functions,” along with the upstream bosses of those things.
Why not a blood test? Urine is close to the pelvis and can be more sensitive than blood (or not as good at homeostasis). Also, patients are happy: one less jab for a blood draw.
In a coordinated national effort, the scientists received 244 urine samples from the masses, labeled them “for the masses” (that is, for the technique called mass spectrometry), blasted them to smithereens — smithereens ordered by mass and charge, for identification — and loaded the data onto the Proteome Discoverer version 2.2.
What did they find?
The levels of nine proteins were different between people with UCPPS and healthy controls.
There were parts of the scaffolds in between cells, and proteins involved in inflammation. The researchers found proteins known for increasing bleeding (previously implicated in UCPPS), for reducing the migration of immune cells, and for the development of epithelial tissue — the lining around blood vessels and organs or their cavities. They also found proteins that work in the postal service of cells, the Golgi.
But what if these protein patterns were due to chronic pain generally, not uniquely UCPPS?
The scientists ran comparisons with people with other chronic pain diseases, and three proteins stood out uniquely in UCPPS. Next, the team wants to conduct a larger study to see if these unconventional fingerprints correlate with disease severity or duration.
Froehlich said he would be “tickled” if other researchers mined the open data to help people with chronic pain diseases. The growing global burden of ME/CFS includes an estimated 46% of people with long COVID-19 who meet criteria for the disease.
Froehlich calls corresponding author Marsha Moses a “powerhouse” behind this research.
He also credits his mother. After completing a Ph.D. on proteins in breast milk (“My mom was a midwife”), Froehlich pivoted to a fluid with its own sort of richness. He simply changed streams.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles
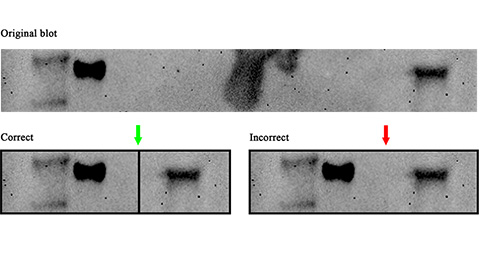
Avoiding common figure errors in manuscript submissions
The three figure issues most often flagged during JBC’s data integrity review are background signal errors, image reuse and undeclared splicing errors. Learn how to avoid these and prevent mistakes that could impede publication.
Ragweed compound thwarts aggressive bladder and breast cancers
Scientists from the University of Michigan reveal the mechanism of action of ambrosin, a compound from ragweed, selectively attacks advanced bladder and breast cancer cells in cell-based models, highlighting its potential to treat advanced tumors.
Lipid-lowering therapies could help treat IBD
Genetic evidence shows that drugs that reduce cholesterol or triglyceride levels can either raise or lower inflammatory bowel disease risk by altering gut microbes and immune signaling.
Key regulator of cholesterol protects against Alzheimer’s disease
A new study identifies oxysterol-binding protein-related protein 6 as a central controller of brain cholesterol balance, with protective effects against Alzheimer’s-related neurodegeneration.

From humble beginnings to unlocking lysosomal secrets
Monther Abu–Remaileh will receive the ASBMB’s 2026 Walter A. Shaw Young Investigator Award in Lipid Research at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

Chemistry meets biology to thwart parasites
Margaret Phillips will receive the Alice and C. C. Wang Award in Molecular Parasitology at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

