Debunking common myths about arthritis
Arthritis causes pain, swelling and inflammation of one or multiple joints. It’s not a single disease but an umbrella term used to refer to a wide array of conditions. It’s one of the most widespread health conditions in the nation.

There are more than 100 types of arthritis, of which osteoarthritis is the most common. Osteoarthritis, also known as degenerative joint disease, occurs over time due to wear and tear of cartilage that protects the ends of the bones. Although osteoarthritis can damage any joint, the disorder most commonly affects joints in the hands, knees, hips and spine.
There are also inflammatory forms, such as rheumatoid arthritis; psoriatic arthritis; and the arthritis associated with ankylosing spondylitis, lupus and gout. In those cases, inflammation is caused by an overactive immune system that attacks connective tissues. (Learn more about autoinflammatory arthritis.)
In the United States, an estimated 58.5 million individuals are gripped with arthritis — the leading cause of disability. More than 50% of this population fall in the working age group (18 to 64 years).
Despite how common this condition is, there are several myths that persist, making it confusing for patients seeking to relieve their symptoms and to improve their quality of life. This article aims at debunking these long-held myths and getting your facts straight!
Myth #1: Arthritis is an old-age disease and cannot affect children.
Fact: Arthritis is more common in older adults, but there are several types that can affect both children and young adults.
Juvenile idiopathic arthritis (also known as childhood arthritis or juvenile rheumatoid arthritis) is the most common type of arthritis among children and can cause permanent physical damage to joints. According to Cleveland Clinic, one in 1,000 children (or about 300,000 children in the U.S.) are affected.
Myth #2: All joint pain is arthritis.
Fact: There are many conditions — such as tendonitis, bursitis and other soft-tissue injuries — that cause joint pain and have a pain profile similar to that of arthritis. Hence, it is of utmost importance to get an accurate medical diagnosis, preferably by a rheumatologist, before treating any kind of joint pain.
Myth #3: When you start experiencing joint pain, you should wait to see if it goes away on its own.
Fact: False! Diagnosing and treating arthritis at its early stage not only can save your joints but also save you from damage to vital organs. Certain forms, such as rheumatoid arthritis, can damage skin, eyes, lungs, blood vessels, the brain and the heart. It is important to determine which type of arthritis you have right away, because treatment varies and starting the correct treatment can be the key to preventing permanent damage.
Myth #4: Arthritis symptoms cannot be improved.
Fact: There currently isn’t a cure for arthritis. However, treatment focuses on relieving symptoms and improving joint function. Working with an arthritis expert can help.
Depending upon the type of arthritis, certain medications can reduce pain and inflammation. Osteoarthritis often is treated with pain-reducing medications, physical activity, weight loss (if the person is overweight) and self-management education.(Learn more about treatment.) Inflammatory disorders are treated with disease-modifying antirheumatic drugs that suppress the immune system.
Heat and cold treatment and assistive devices, such as walkers, braces and gloves, also can help.
Myth #5: Exercising will worsen your condition.
Fact: Exercise can help increase strength, motion and flexibility and reduce pain and swelling. Inactivity can cause the symptoms to worsen, thus increasing both pain and swelling. Before you enroll in any exercise program, it is also important to know what your limits are and what level of exercise you can benefit from.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles
Cracking cancer’s code through functional connections
A machine learning–derived protein cofunction network is transforming how scientists understand and uncover relationships between proteins in cancer.

Gaze into the proteomics crystal ball
The 15th International Symposium on Proteomics in the Life Sciences symposium will be held August 17–21 in Cambridge, Massachusetts.
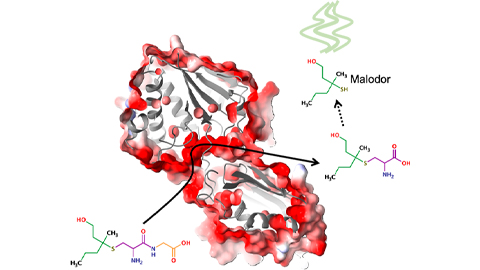
Bacterial enzyme catalyzes body odor compound formation
Researchers identify a skin-resident Staphylococcus hominis dipeptidase involved in creating sulfur-containing secretions. Read more about this recent Journal of Biological Chemistry paper.

Neurobiology of stress and substance use
MOSAIC scholar and proud Latino, Bryan Cruz of Scripps Research Institute studies the neurochemical origins of PTSD-related alcohol use using a multidisciplinary approach.
Pesticide disrupts neuronal potentiation
New research reveals how deltamethrin may disrupt brain development by altering the protein cargo of brain-derived extracellular vesicles. Read more about this recent Molecular & Cellular Proteomics article.

A look into the rice glycoproteome
Researchers mapped posttranslational modifications in Oryza sativa, revealing hundreds of alterations tied to key plant processes. Read more about this recent Molecular & Cellular Proteomics paper.

