Brain Injury Awareness Month 2021
March is Brain Injury Awareness Month, a time to bring public attention to an issue affecting millions of people in the U.S. every year. The Brain Injury Association of America leads this campaign with the purpose of destigmatizing brain injury, empowering those who have survived a brain injury, and promoting the many types of support available.
Many ways to injure your brain
According to the BIAA, a person in the U.S. sustains a brain injury every nine seconds, culminating in more than 3.5 million injuries each year. There are several clinical classifications for brain injuries. Doctors refer to injuries that do not occur at or around the time of birth and are not genetic or degenerative as an acquired brain injury. An ABI can be either a nontraumatic or a traumatic brain injury, depending on the injury’s inciting source.
Nontraumatic brain injuries include:
- infectious disease
- electric shock
- toxic exposure
- metabolic disorders
- neurotoxic poisoning
- lack of oxygen
- drug overdose
Traumatic brain injuries include:
- car and motorcycle accidents
- sports injuries
- abusive head trauma
- gunshot wounds
- workplace injuries
The BIAA also reports that, in the U.S., about 2.8 million people sustain a TBI annually, with some 280,000 resulting in hospitalizations. Of those injuries, about 50,000 are fatal, meaning there are approximately 155 deaths every day from TBI-related injuries. One in every 60 people has a TBI-related disability, culminating in around 5.3 million people total.
There are three levels of TBI severity: mild, moderate and severe. Doctors determine the severity of the injury using the Glasgow coma scale, which examines motor response, verbal ability and eye opening — ranking patient responses with a total score between 3 and 15. A mild TBI lands on the higher side of the scale, whereas a severe TBI results in a lower score.
Risk factors and vulnerable patient populations
Falls are a major cause of brain injury, resulting in 40.5% of all TBIs. This places adolescents, young adults and elderly patients at the highest risk for TBI-related injuries.
The Hope Network, a nonprofit service provider for people with brain and spinal cord injuries, reports that elderly patients (age 65 and older) are at greater risk for hospitalization and death after sustaining a TBI. The Centers for Disease Control and Prevention supports this claim, citing a 17% nationwide increase in fall-related TBI deaths between 2008–2017, occurring most often in people age 75 years or older.
Men are two times more likely to suffer a TBI-related injury than women. They are also more likely to become hospitalized or die from their injuries. The BIAA attributes this difference to male involvement in higher-risk behaviors that can cause the injury, affect recovery and increase the risk of recurring injuries. Further, gender differences in societal expectations of self-care after injury and the rate of recovery may potentiate negative patient outcomes for men. The fact that male patients ignore medical advice more often, opting to leave the hospital earlier than recommended after injury, plainly illustrates this phenomenon.
Current research in TBIs
TBIs are an active area of study for neuroscience researchers. The National Institute of Neurological Disorders and Stroke emphasizes funding support for laboratories investigating the molecular and clinical factors of TBIs. Below are a few TBI-focused research highlights from American Society for Biochemistry and Molecular Biology journals.
TBI-related dementia: Patients who sustain multiple concussions or a moderate TBI are at risk for a type of dementia that presents at an early age. Scientists are still learning how TBI and dementia are linked on a molecular level. This study in the Journal of Biological Chemistry identifies a toxic form of a microtubule protein, called tau, in rats’ brains post-TBI. Tau plays a major pathological role in several types of dementia. These findings reveal a potential connecting factor involved in TBI-related dementia and an early-detection marker for patients.
Inactivating calpain-1 for TBI treatment: A TBI can cause brain-cell death and tissue degeneration, potentially leading to many negative clinical symptoms for the patient, depending on the severity of the injury. One therapeutic approach involves targeting the molecular pathway that controls cell death. Calpains are an essential protein that regulates this process, prompting researchers to investigate whether silencing calpains minimizes TBI-related brain damage. Their results showed therapeutic promise, with observed reductions in cell death and tissue degeneration when silencing calpain-1. The study was published in JBC.
Fixing a dysfunctional mitochondria: Mitochondria are an essential part of cell metabolism — any disruption in their interworking can lead to a host of cell issues. A cellular membrane component called sphingolipids are involved in brain cell signaling, mitochondrial function and cell death. Sphingolipids are rapidly metabolized in the mitochondria by key enzymes, such as neutral ceramidase (NCDase) and sphingosine kinase 2 (SphK2). Researchers discovered that TBIs significantly alter sphingolipid metabolism by activating NCDase and suppressing SphK2. Unchecked activation of NCDase leads to an accumulation of sphingosine, leading to mitochondrial dysfunction and cell death. This study, published in JBC, successfully demonstrates how decreasing NCDase activation restores sphingolipid metabolism and decreases TBI-induced damage.
CRMP2 protects against TBI-induced damage: The brain relies heavily on a neurotransmitter, called glutamate, as its primary communication “on” switch. Releasing glutamate activates neighboring brain cells, allowing the transmission of important messages throughout the brain. However, too much glutamate causes brain damage through a pathological process called excitotoxicity. Neurological disorders and TBIs can cause cell death by overactivating the glutamatergic system. This study in JBC demonstrates how stimulating the expression of a neuronal protein called CRMP2 can protect against brain-cell death in excitotoxic conditions.
Cerebral ketone metabolism as a therapeutic strategy: Neurons use glucose as a primary energy source, metabolizing it to power their many functions. When a TBI occurs, it causes neurons to metabolize glucose less, depleting energy levels. In this thematic review in the Journal of Lipid Research, the authors argue for the use of ketone bodies as an energy replacement because they are a natural energy alternative to glucose. This paper discusses several studies demonstrating improved recovery from a TBI using a ketogenic diet intervention.
Protecting mitochondrial function post-TBI: The sphingolipid recycling pathway refers to how the product of sphingolipid catabolism, sphingosine, is recycled into a metabolite called ceramide. As mentioned above, mitochondrial function depends on preventing sphingosine accumulation. Researchers writing in JLR focused on an important enzyme in the recycling pathway, acid sphingomyelinase. They found that activating ASM promotes sphingosine accumulation in the mitochondria. Increased sphingosine levels may contribute to functional abnormalities in the first week post-TBI.
TBI and Parkinson’s disease: Scientists are using large-scale biological techniques to understand better the molecular impact of TBI and how this connects to other neurological disorders. This study in the journal Molecular & Cellular Proteomics investigates changes in protein expression throughout several brain regions after a brain injury. The researchers found elevated expression of major proteins previously implicated in Parkinson’s disease. A pathological hallmark of Parkinson’s, called alpha-synuclein, may provide a linking component between TBIs and Parkinson’s. These findings provide evidence supporting greater PD risk in TBI patients.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles
From the Journals: JBC
How cells recover from stress. Cancer cells need cysteine to proliferate. Method to make small membrane proteins. Read about papers on these topics recently published in the Journal of Biological Chemistry.

ASBMB names 2025 JBC/Tabor Award winners
The six awardees are first authors of outstanding papers published in 2024 in the Journal of Biological Chemistry.
Pan-kinase inhibitor for head and neck cancer enters clinical trials
A drug targeting the scaffolding function of multiple related kinases halts tumor progression.

Sweet secrets of sperm glycosylation
Scientists from Utrecht University uncover similar glycosylation patterns in sperm from bulls, boars and humans, distinct from those found in blood across species. These findings may improve IVF and farming techniques.
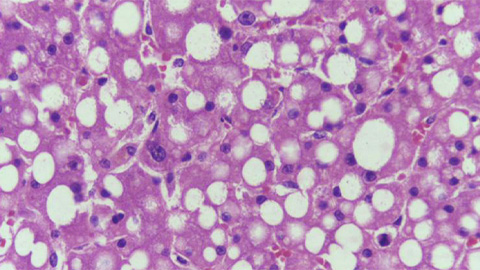
From the Journals: JLR
Promising therapeutic candidate for steatosis. Unique lipid profiles in glycogen storage disease. Microglial lactic acid mediates neuroinflammation. Read about these recent papers.
Meet Robert Helsley
The Journal of Lipid Research junior associate editor studies chronic liver disease and was the first in his family to attend college.

