From the JBC archives: Madness, indoles and mercury-based cathartics
In a 1907 Journal of Biological Chemistry article, J. Harvey Borden, a clinical assistant at the New York Pathological Institute, sought to resolve an ongoing question of whether indole, a bacterial molecule in the gut, could cause insanity if overproduced . This may sound outlandish or archaic now, but at the turn of the 20th century, it was a natural continuation of ongoing research.
A decade earlier, another scientist reported that bacteriain the colon produce significant amounts of indole, and this may have drawn attention because indole production was a standard way of distinguishing cholera spirilla from other spirilla. If indole was related to disease, and the indole being produced in the bowels wasn’t causing physical symptoms, could it be responsible for psychiatric symptoms?
Findings showing a relationship between indole and insanity began to circulate, and soon highly regarded members of the field such as Otto Folin weighed in with their own investigations. We can imagine that anyone doing related research, like Borden, would be tempted to add decisive work to the conversation.
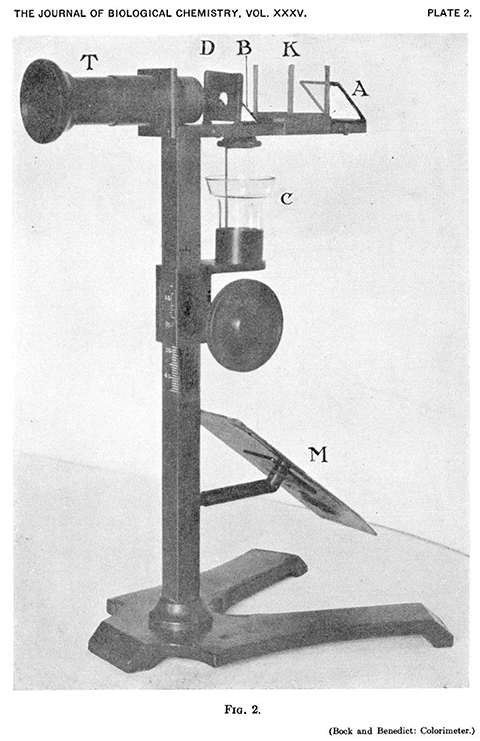
Some of the experimental fervor surrounding this question was probably stoked by the fact that indole accumulation could be approximated with a noninvasive colorimetric assay. The indole metabolite indoxyl is excreted in urine and yields blue indigo dye when oxidized. Patient’s urine could be treated with a few widely available reagents and assessed for its shade of blue. The bluer the sample, the more indoxyl being produced.
Researchers performed this analysis in an assortment of ways with institutionalized psychiatric patients, and as a result, indole was linked to afflictions including epilepsy, catatonia, migraine, manic-depressive episodes, and aptly, “the blues.”
Borden’s way
While watching all this unfold, Borden noted that the literature was in stark disagreement about the effect. Some studies showed a clear link between indole and insanity while others showed no connection whatsoever. As can also be seen from the list above, no two studies seemed to agree on the type of insanity caused by excess indole.
In designing his investigation, Borden began by comparing the methodology of those studies that connected indole with insanity and those that didn’t. He noticed one thing in particular: The studies that reported a positive correlation typically relied on qualitative color assessments while those reporting no relationship favored quantitative measurement.
Borden’s system for categorizing the original hue of samples illustrates the problem with relying on qualitative assays. Distinguishing the colors “light amber” from “straw” would be difficult even if faced with the samples, let alone reading their description in a manuscript. Results couldn’t be compared easily between studies, and even those that converted qualitative descriptions to measured amounts of indoxyl might suffer from inconsistent or unreliable standard solutions.
Borden developed a slightly more precise method of estimating indoxyl content. All of a patient’s urine was collected over 24 hours, and the purified sample was diluted until its shade of blue matched that of a one milligram per liter solution of indigo. By recording the amount of diluent required, the amount of indoxyl in the original sample could be calculated.
With this assay and the prudent decision to include a control group of nonhospitalized subjects, Borden concluded that no connection between indole and mental illness could be identified. For both acute and chronic cases of insanity, the estimated indole did not exceed that of the control group of healthy individuals. He further noted, perhaps just as importantly, that such studies were inherently difficult and destined to be noisy. The habits and diets of the patients were often erratic, the classification of mental illnesses tended to be hazy and the means of measuring indole were indirect.
The ‘cure’
What practical impact might this result have had? At the end of his article, Borden lists 37 case histories of the examined patients. The amount of identifying information in these histories is a bit jarring, and it provokes curiosity about how Borden’s findings might affect these patients.
What does it mean for 45-year-old Mary Straits, admitted in 1905 for manic-depressive insanity, that her illness doesn’t stem from an accumulation of indole? In the clinical environment of that era, this negative result might have been the best outcome due to the treatments available. If research had shown that indole in the bowel caused nervous disorders, then clearing the bowel would be the most effective means of clearing the mind. Cathartics were the available means of doing this, and at the time of publication one drug served as the gold standard.
Borden recounts the findings of a study that did assert some relationship between indole and insanity: “They took some calomel, the indoxyl disappeared, the world once more looked bright, and it seemed as though the indoxyl must have been at least one factor in causing the depression.”
Through the late 18th and early 19th centuries, calomel was the flagship medicament of what became known as the “heroic” school of medicine in which treatment largely consisted of purgatives and bleeding.
Calomel is a mineral of mercury chloride. It functioned as a cathartic, but just as well if not better as a poison. Patients experienced vomiting and gastric pain, ulcers, loss of their teeth and a variety of other symptoms attributed to mercury poisoning. By the late 19th century, public distaste for the brutal effects of calomel had bolstered alternative medicine and even inspired a genre of poetry:
He then weighs out the fatal grains-
I think, mam, this will cure the pains-
Once in three hours, at sound of bell
Give him a dose of Calomel.
The man in death begins to groan,
The fatal job for him is done
His soul is forced to heaven or hell,
a sacrifice to Calomel.
The medical community was dedicated to the drug, however, and prescribed it into the 20th century. When treating nervous disorders stemming from stagnant bowels, a physician’s first thought might well be calomel. Because mental illness is often chronic, patients might receive long-term treatment that was bound to be agonizing if not fatal.
Wrong, but also right
What have we learned about indole and mental illness since Borden published his article? This line of inquiry never completely faded away, and more recent results show Borden may not have been entirely correct.
More than a decade ago, researchers found that some bacteria synthesize indole from tryptophan via the activity of tryptophanase, and thereafter this indole serves as a signaling molecule that can guide a multitude of processes related to resilience, virulence and communal interactions for gut microbiota . This signaling does appear to affect the mental state of mammalian hosts: A study has linked E. coli’s production of indole to anxiety-related behaviors in rats , and other researchers connected indoxyl sulfate abundance in human serum (we moved on from urine) to functional MRI signatures related to anxiety .
Borden was plainly wrong, but it could be argued that his most important insight was correctly identifying the inherent murkiness of the whole field of study.
Research since Borden’s time has deepened the complexity of the molecular relationship between the gut and brain. Far from being an isolated player, indole is one of several tryptophan metabolites that can perturb mental states. Human metabolism can convert tryptophan into serotonin and kynurenine, which both have demonstrated impacts on depressive symptoms . Bacterial metabolism and indole production could easily shunt dietary tryptophan away from these biosynthetic pathways, but the degree to which this happens would depend on the size and composition of the microbial community.
On a more fanciful note, we now know that the hallucinogenic indolethylamines psilocybin, N,N-dimethyltryptamine, and bufotenin trace their biosynthetic origins to tryptophan . A number of groups in the 1960s investigated the occurrence of bufotenin in the urine of schizophrenic patients , but this thread has, probably sensibly, been abandoned over the years.
We can see that our brain activity is susceptible to minute changes in the structure of tryptophan, and that an assortment of these compounds can be floating around depending on diet, microbiota and endogenous metabolism. Whether individual metabolites are measured with colorimetric assays or gas chromatography, it’s unlikely that we could identify a single axis around which mental states revolve.
Such complexity means we must be careful how we select our questions. Among the many interesting paths we could follow, are any clinically relevant outside of highly controlled conditions? Are there feedback loops between brain states, immune responses and microbiota? If so, are they periodic? Does the effect of bacterial signaling on host mood offer an advantage to bacterial populations, or is this a spandrel in Gould and Lewontin’s sense of the word?
Researchers may be working on these questions already. And perhaps more mechanisms are waiting to be discovered to add a new chapter to this century-long journey.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

Defining a ‘crucial gatekeeper’ of lipid metabolism
George Carman receives the Herbert Tabor Research Award at the ASBMB Annual Meeting, March 7–10, just outside of Washington, D.C.
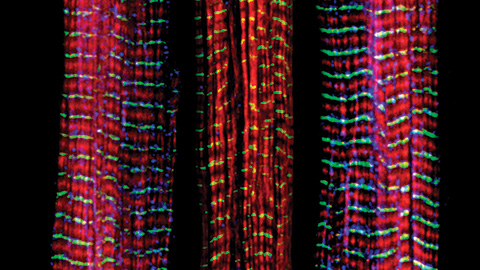
The science of staying strong
Muscles power every movement, but they also tell the story of aging itself. Scientists are uncovering how strength fades, why some species resist it and what lifestyle and molecular clues could help preserve muscle health for life.
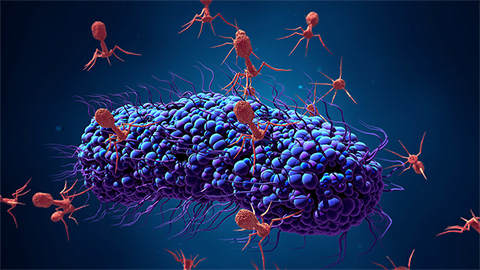
Bacteriophage protein could make queso fresco safer
Researchers characterized the structure and function of PlyP100, a bacteriophage protein that shows promise as a food-safe antimicrobial for preventing Listeria monocytogenes growth in fresh cheeses.

Building the blueprint to block HIV
Wesley Sundquist will present his work on the HIV capsid and revolutionary drug, Lenacapavir, at the ASBMB Annual Meeting, March 7–10, in Maryland.
Gut microbes hijack cancer pathway in high-fat diets
Researchers at the Feinstein Institutes for Medical Research found that a high-fat diet increases ammonia-producing bacteria in the gut microbiome of mice, which in turn disrupts TGF-β signaling and promotes colorectal cancer.

Mapping fentanyl’s cellular footprint
Using a new imaging method, researchers at State University of New York at Buffalo traced fentanyl’s effects inside brain immune cells, revealing how the drug alters lipid droplets, pointing to new paths for addiction diagnostics.

