Patients lose weight in trials of schizophrenia drug
There remains a significant need for new therapeutic options for the treatment of patients with, often debilitating, psychiatric disorders. Current therapies are frequently associated with side effects, including unexplained weight gain in about one-third of patients. Breakthroughs in brain research and the discovery of potential novel drug targets are leading to the development of a new generation of candidate therapies that are providing early signs of hope for these patients.

Hence, when Michal Tomaszewski, an associate principal scientist at Merck & Co., and his team learned from their colleagues that patients treated with an investigational antipsychotic medicine lost weight in a Phase 2a clinical trial, they knew they needed to better understand the mechanism of weight decline.
In their recent paper published in the Journal of Lipid Research, the researchers record the results of their investigation, which showed the antipsychotic drug, a phosphodiesterase-10A, or PDE10A, inhibitor, significantly reduced the amount of stored fat in both white and brown adipose tissue in mice.
“Studying this transition lets us better understand the effect of the PDE10A inhibitor treatment on metabolism,” Tomaszewski said.
When white adipose tissue exhibits increased vasculature and metabolism, it is an indicator of its conversion into brown adipose tissue, or BAT. BAT cells burn up fat as heat energy, and increasing levels of these cells are often accompanied by weight loss. The researchers observed an increase in blood vessels and blood flow in white adipose tissue compared to a control.
“Specifically, the white adipose tissue showed enhanced blood vessel growth and increased consumption of fat for energy,” Tomaszewski said. “These changes were consistent with a transition to brown adipose tissue, which is known to be important in how we store and use energy, and therefore how we gain and lose weight.”
To see these effects, the researchers used magnetic resonance imaging in a novel way that helped them characterize the physiological changes in adipose tissue in response to the PDE10A inhibitor. They observed the transition of white adipose tissue into brown adipose tissue, which has higher energy metabolism. This explained the weight loss seen in PDE10A inhibitor-treated mice.
“This magnetic resonance imaging application provided detailed insights into metabolism and physiology not available using most other methods,” Tomaszewski said. “This technique may, in the future, be applied more broadly to evaluate the response of adipose tissue to additional experimental drug candidates.”
Tomaszewski believes this work resulted in multiple benefits. “Although imaging of mice in vivo was the focus of the study and made it possible to visualize the changing nature of the adipose tissue,” he said, “we were also able to perform comprehensive validation using genetic and protein analysis, which all aligned to reinforce our conclusions.”
Tomaszewski said he is optimistic that the magnetic resonance imaging methods used in this work “can be scaled to evaluate similar metabolic changes in people.”
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

The data that did not fit
Brent Stockwell’s perseverance and work on the small molecule erastin led to the identification of ferroptosis, a regulated form of cell death with implications for cancer, neurodegeneration and infection.

Building a career in nutrition across continents
Driven by past women in science, Kazi Sarjana Safain left Bangladesh and pursued a scientific career in the U.S.
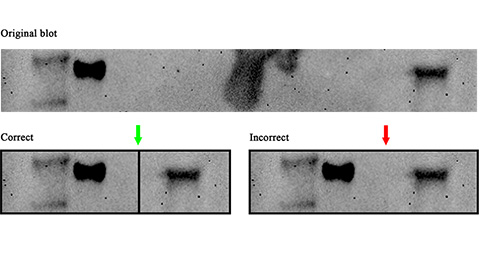
Avoiding common figure errors in manuscript submissions
The three figure issues most often flagged during JBC’s data integrity review are background signal errors, image reuse and undeclared splicing errors. Learn how to avoid these and prevent mistakes that could impede publication.
Ragweed compound thwarts aggressive bladder and breast cancers
Scientists from the University of Michigan reveal the mechanism of action of ambrosin, a compound from ragweed, selectively attacks advanced bladder and breast cancer cells in cell-based models, highlighting its potential to treat advanced tumors.
Lipid-lowering therapies could help treat IBD
Genetic evidence shows that drugs that reduce cholesterol or triglyceride levels can either raise or lower inflammatory bowel disease risk by altering gut microbes and immune signaling.
Key regulator of cholesterol protects against Alzheimer’s disease
A new study identifies oxysterol-binding protein-related protein 6 as a central controller of brain cholesterol balance, with protective effects against Alzheimer’s-related neurodegeneration.

