Disappointed — by cancer
After spending a day with a bad cold and a pounding headache, I found myself standing in the shower at 1 a.m. rinsing out the drainage from a ruptured eardrum.
It was the sort of thing I’d comforted my toddler through numerous times. I could hardly believe my robust adult immune system had succumbed to a little kid’s ailment — an ear infection!
I was scheduled to leave town for the next week on a series of seminar visits and figured an immediate trip to the doctor’s office was warranted. My nurse-clinician, Katie, prescribed amoxicillin. She also gently suggested I go get that key lime-shaped thing lodged in my right breast — the one I had mentioned noticing about a month before — checked out and wrote an order for a mammogram. It was probably nothing, probably just a cyst, she said, but just to be safe, I should get it looked at right away. And the radiology department had really good, free coffee — so why not stop in on the way to work?
 Jennifer DuBois works with senior Ph.D. student Arianna Celis,
Jennifer DuBois works with senior Ph.D. student Arianna Celis,who says, “We take a lot of joy in what we do and in each other.”Photo by Kelly Gorham
I set the mammogram order aside and went on my seminar trip, feeling around the bloating key lime while sitting in my hotel room, though I was still pretty sure it was just a cyst. I promptly scheduled a trip to the radiology department after my return and enjoyed a free chai latte in the ladies-only waiting room, wearing a fluffy pink robe. This wasn’t so bad, I thought.
I was called into the exam room. As a biochemist and spectroscopist by training, the mammography machine to me seemed strangely clunky and ill-designed. A spritely young woman posed me like a Greek statue while she squashed flesh between paddles, first left, then right, each time instructing me not to breathe. She would not read the mammogram herself, but she assured me the radiologist would before I went home that day.
She sent me back out to the waiting room, but before I could get a refill on the free latte, I was unexpectedly called into the next room for an ultrasound. A mother of three, I was very familiar with this device, though I had never had it applied above the waist.
The radiologist introduced himself and said the mammogram warranted some follow-up. He rolled the instrument’s paddle around and over and over my right breast — stopping and taking images, measuring, and uttering the occasional “hmm” or asking the technician to take down a number.
After about 15 quiet minutes of this, I asked, “So, doc, what is it — boy or girl?” I winced and immediately wondered how many nervous women had made the same joke. He looked me in the eye. He knew I was a scientist, and he discerned my preference for technical descriptions, which he proceeded to give. But the way he summed it up was far more memorable: “You have something inside you which is big and mean. We will need the biopsy for sure, but what you have is almost certainly cancer. I am so sorry to give you this news.”
In the dressing room, where I changed out of the fluffy pink robe, I texted my husband that one word: “cancer.”
In biochemistry circles as well as among the general public, we have become accustomed to the idea that cancer is not one but rather many diseases. But still, the word and the strangely unitary diagnosis persists. At that moment, I was not sure whether I was facing merely a highly complicated wart removal or something far more difficult and life-threatening. All I had to go on was that word, “cancer.”
It was with unexpected excitement that I scheduled the biopsy that would give me a more specific diagnosis for the next day. I felt excitement because, as a biochemist, I expected the biopsy and its analysis to give me concrete answers while putting the awesome power of my field on full display. I had come of age during the era in which major cell-signaling pathways were unraveled; the human genome sequenced; databases of single-nucleotide polymorphisms assembled; and microarray, high-resolution mass spectroscopy and chemical genetics technologies blossomed. I was looking forward to seeing the pile of data that my biopsy would produce.
So how vast was the microarray database to which my tumor cells were compared? Actually, microarray data were not measured. How many PCRs were run? None. How many biomarkers were assayed? 30? 40? Try three, all by simple immunohistochemical stains painted on the surfaces of the excised masses.
Of those three markers, only two have any real treatment potential: overexpressed estrogen receptor (ER for short) or epidermal growth factor receptor, or EGFR. Even now that I am in the treatment phase, I have had no blood-borne markers, no circulating tumor cells assayed. The efficacy of my treatment is being assessed only statistically — by comparing me to the thousands of others who have received the same chemotherapy regimen before me.
Half of that regimen consists of doxorubicin (brand name Adriamycin), an anthracycline-based natural product from Streptomyces that initially received Food and Drug Administration approval in 1974. In my lab, we have been studying part of the biosynthetic pathway of its precursor compound, in part because of the importance of its use in a decidedly nonmedicinal application: breaking down wood pulp ( 1).
My new graduate student demonstrated its oxidizing power to me in stomach-churning fashion when she brought a test tube full of the sickly red Adriamycin core mixed with what looked like melted plastic. She had been attempting to measure the redox potential of her solution with an epoxy-coated electrode, and the precursor compound had dissolved the coating clean off the underlying glass.
And here I am, having 84 milligrams of this nasty stuff pumped into me by a special, personal-protective-equipment-clad oncology nurse every two weeks!
The second chemotherapeutic I get is Cytoxan, a cyclophosphamide DNA alkylator with FDA approval dating to 1959.
This was a far cry from the personalized medicine I had expected. What had become of all those fabulous papers, talks and poster sessions I’d seen over the years? It dawned on me that my initial, gut response to my cancer diagnosis and treatment plan had not been so much fear or dread but rather a surprising sense of professional disappointment.
But that’s only the first half of the story.
My biopsied (and now surgically removed) tumor and lymph nodes turned out to be positive for one of those three biomarkers: EGFR, better known in oncology circles by its gene locus name, HER2 ( 2). Seminal discoveries related to HER2 in the mid-1980s made by Dennis Slamon and Stuart Aaronson of the University of California, Los Angeles, and Icahn Mount Sinai schools of medicine, respectively, linked its overexpression to rapid cell proliferation in about 25 percent of breast cancers. I remember learning about this way back in the mid-1990s in an undergraduate class I took called “Oncogenes.”
Antibody-based, anti-HER2 therapeutics subsequently were developed by Genentech, eventually receiving FDA approval in 2006. The resulting drug, marketed as Herceptin, has been a game-changer for people like me with a diagnosis of highly aggressive, HER2-overexpressing (Her2+) breast tumors. Given after or in combination with conventional cytotoxic chemotherapeutics, Herceptin has had impressive, even fully curative and recurrence-free outcomes for patients like me who just a short time ago would have had very much darker prospects.
In 2012, a second monoclonal antibody (pertuzumab, marketed as Perjeta) was approved for use against Her2+ cancers.
In the meantime, a series of other cancers — of the ovary, endometrium, bladder, lung, colon, head, neck and esophagus — have been shown to overexpress HER2 and are consequently susceptible to targeted immunotherapies like Herceptin and Perjeta. Along with Gleevec, the first targeted cancer therapy to receive FDA approval (2001), these drugs have revolutionized treatments for those lucky enough to have cancers that are vulnerable to them.
Gleevec, developed by Novartis, represents a brilliant success story for small-molecule medicinal chemistry. It targets the unnatural, cell-proliferation-associated tyrosine kinase BCR-ABL, which forms when a piece of chromosome 22 fuses to the end of chromosome 9 (generating the so-called “Philadelphia chromosome”). Like Herceptin and Perjeta, Gleevec has been nothing short of a wonder drug, in this case for patients with forms of leukemia that previously would have left little cause for hope.
As amazing as these targeted therapies are, we may still ask why there aren’t more of them. By the same token, why, with so many stunning advancements in diagnostics, aren’t these methods more widely applied?
My oncologist suggested that diagnostics generally are not used unless they are associated directly with a specific treatment option, of which there are still just a few. And with the time involved in translating basic discovery through a sharply winnowed pipeline into a safe, well-vetted treatment (about 20 years in the case of both Herceptin and Gleevec), we should expect such treatments to emerge at a slow pace.
So what’s a scientist working on medically relevant basic research to do?
Be patient. Recognize that translational research and medicine will catch up eventually with, and fully exploit, the explosive pace of discovery that molecular and cellular biology has enjoyed for the past 40 years. Science may be lapping medicine for the time being, but that won’t always be the case. In the meantime, we need to keep working to make a difference for the millions of people who still await a cure.
It’s now two months on from the ear infection that led me to a diagnosis of breast cancer. A few days ago, I had a dream. I was standing on a curb when a red double-decker bus, the kind you see in London, pulled up and opened its door. The driver called to me menacingly, “It’s time for you to come with us. It’s time for you to come sing with the choir.” As I began to step off the curb, my husband drove up beside him, our young kids in the backseat. “She’s not going with you,” he insisted. “She’s coming with us.” And away we sped, happy and safe.
I will receive Herceptin along with Taxol in the next phase of my treatment. My doctor says my long-term prospects are excellent. I know that I am incredibly lucky just a short time ago would have had very much darker prospects.
References
1. http://www.jbc.org/content/291/34/17816
2. https://pdb101.rcsb.org/motm/126
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Opinions
Opinions highlights or most popular articles

Women’s health cannot leave rare diseases behind
A physician living with lymphangioleiomyomatosis and a basic scientist explain why patient-driven, trial-ready research is essential to turning momentum into meaningful progress.

Making my spicy brain work for me
Researcher Reid Blanchett reflects on her journey navigating mental health struggles through graduate school. She found a new path in bioinformatics, proving that science can be flexible, forgiving and full of second chances.

The tortoise wins: How slowing down saved my Ph.D.
Graduate student Amy Bounds reflects on how slowing down in the lab not only improved her relationship with work but also made her a more productive scientist.
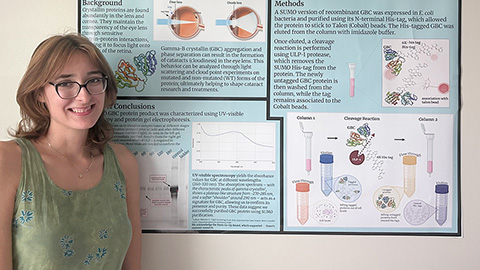
How pediatric cataracts shaped my scientific journey
Undergraduate student Grace Jones shares how she transformed her childhood cataract diagnosis into a scientific purpose. She explores how biochemistry can bring a clearer vision to others, and how personal history can shape discovery.

Debugging my code and teaching with ChatGPT
AI tools like ChatGPT have changed the way an assistant professor teaches and does research. But, he asserts that real growth still comes from struggle, and educators must help students use AI wisely — as scaffolds, not shortcuts.

AI in the lab: The power of smarter questions
An assistant professor discusses AI's evolution from a buzzword to a trusted research partner. It helps streamline reviews, troubleshoot code, save time and spark ideas, but its success relies on combining AI with expertise and critical thinking.

