The uses of metabolic adversity
Blurred vision was the first sign that something was wrong. The front row of the freshman chemistry class I was teaching looked strangely fuzzy. Then, over the next few days, I was gripped by an unquenchable thirst and was constantly fatigued. Seemingly overnight I lost eight pounds. I recognized the symptoms of diabetes, but I was young(ish), slim(ish) and an avid kick-boxer. Mine was not the typical diabetic profile.
.jpg) Despite my suspicion that I was experiencing raging hyperglycemia, the diagnosis — “You have diabetes” — was devastating. It marked the beginning of a lifestyle that is an enormous challenge. However, the journey has led me to an increased understanding of biochemistry, has enhanced my teaching and ultimately has cast me in a new role of helping others.
Despite my suspicion that I was experiencing raging hyperglycemia, the diagnosis — “You have diabetes” — was devastating. It marked the beginning of a lifestyle that is an enormous challenge. However, the journey has led me to an increased understanding of biochemistry, has enhanced my teaching and ultimately has cast me in a new role of helping others.
Fortunately, I felt equipped to manage my condition. I teach metabolism to undergraduates using an approach that emphasizes insulin-dependent pathways as a unifying theme and one that offers an everyday context. I knew that carbohydrates, whether whole grain or highly processed, could raise my blood glucose to dangerous levels, so my response to the diagnosis was to reduce greatly carbohydrates in my diet. In addition, I was careful to monitor my blood sugar levels and insulin doses. The result was that my hemoglobin A1c (glycosylated hemoglobin, a measure of blood sugar control), was 5.4 percent, within the normal 4 percent to 5 percent range. My doctor said that I was his “best patient ever” and that I was achieving the blood sugars of a nondiabetic person.
Despite satisfaction with my glycemic control, my physician wanted me to see a dietitian. To my surprise, the dietitian was appalled by my diet. She said, “You have to eat a minimum of 130 grams of carbohydrates a day.” I protested, but she recruited the rest of the medical team to endorse her position: “We all say you have to eat more carbs. The American Diabetes Association gives us these guidelines.” One member of the team said, “I want you to eat chocolate. I want you to enjoy life.”
As someone raised to be cooperative, and because I found it easy to embrace medical advice to eat chocolate, I agreed to eat more carbohydrates. The result was that my HbA1c rose above 7 percent. My blood sugar levels were frequently in the 200 to 300 mg/dl range (far above the normal level of about 85 mg/dl), even when I supplemented with extra insulin. My former dose of seven units of insulin per day increased to 30 units per day. The loss of control was immensely frustrating. My physician attributed my initial success to what is called the diabetes honeymoon. Often, when someone first begins taking insulin, there is a short-lived period during which β-cells seem to recover a bit and secrete insulin. Regardless, it was clear that the dietitian’s approach was not yielding the success I desired. I felt confused and uncertain as to what to do.
I decided to investigate for myself what my best diet should be. I studied the literature, I sought out researchers and physicians, and I attended countless metabolism-related talks. In addition, I connected with hundreds of people with diabetes. The most important contribution to my achieving clarity, however, was evaluating literature based on a molecular understanding of how metabolism works.
In my quest for answers, I found to my surprise that many dietitians and physicians were unable to explain the basis for the dietary recommendations they endorsed. Some did, however, express a desire for a better understanding or review of what they’d once learned. And in the general public, I encountered scores of diabetics and nondiabetics who also wanted tools to make sense of conflicting nutritional information.
I began to use what I had learned not only to expand and improve my teaching and research but also to step into the role of a nutrition explainer. First I was determined to see that none of my students would lack understanding of processes such as gluconeogenesis and the many pathways affected by insulin. I created new lecture topics and problem sets based on diabetes and nutrition applications. My students responded positively and appreciatively. There was a palpable increase in attention in class. Students came to my office to chat about things that they had read. My class evaluations praised the use of nutritional context and often said, “This material could have been rather dull without all these great applications.” I even heard (frequently) “I love metabolism!”
Beyond my student population, I engaged a world of bloggers, physicians and other people with diabetes, many of whom were eager to understand more deeply how things work metabolically. I now find myself being interviewed, quoted in papers, and invited to speak to groups of people, including physicians, who want to deepen their understanding of metabolic pathways. I am asked to share my nutrition-based teaching applications with other professors and with textbook publishers. In these efforts, I try to avoid dispensing nutritional advice; instead, I attempt to show how nutrient composition affects metabolic pathways so that my audience feels better able to evaluate nutritional recommendations.
Five years later, diabetes is still an immense mental and physical challenge, but I am grateful for the insight and tools that my education and training have provided me. Most importantly, if I am able to further the use of molecular science to help others find optimal dietary strategies, and if I can help the next generation, then my adversity will have had a positive outcome.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Opinions
Opinions highlights or most popular articles

The tortoise wins: How slowing down saved my Ph.D.
Graduate student Amy Bounds reflects on how slowing down in the lab not only improved her relationship with work but also made her a more productive scientist.
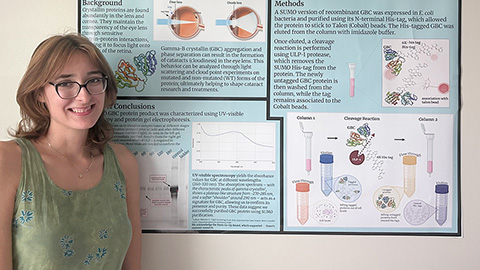
How pediatric cataracts shaped my scientific journey
Undergraduate student Grace Jones shares how she transformed her childhood cataract diagnosis into a scientific purpose. She explores how biochemistry can bring a clearer vision to others, and how personal history can shape discovery.

Debugging my code and teaching with ChatGPT
AI tools like ChatGPT have changed the way an assistant professor teaches and does research. But, he asserts that real growth still comes from struggle, and educators must help students use AI wisely — as scaffolds, not shortcuts.

AI in the lab: The power of smarter questions
An assistant professor discusses AI's evolution from a buzzword to a trusted research partner. It helps streamline reviews, troubleshoot code, save time and spark ideas, but its success relies on combining AI with expertise and critical thinking.

How AlphaFold transformed my classroom into a research lab
A high school science teacher reflects on how AI-integrated technologies help her students ponder realistic research questions with hands-on learning.
Writing with AI turns chaos into clarity
Associate professor shares how generative AI, used as a creative whiteboard, helps scientists refine ideas, structure complexity and sharpen clarity — transforming the messy process of discovery into compelling science writing.

